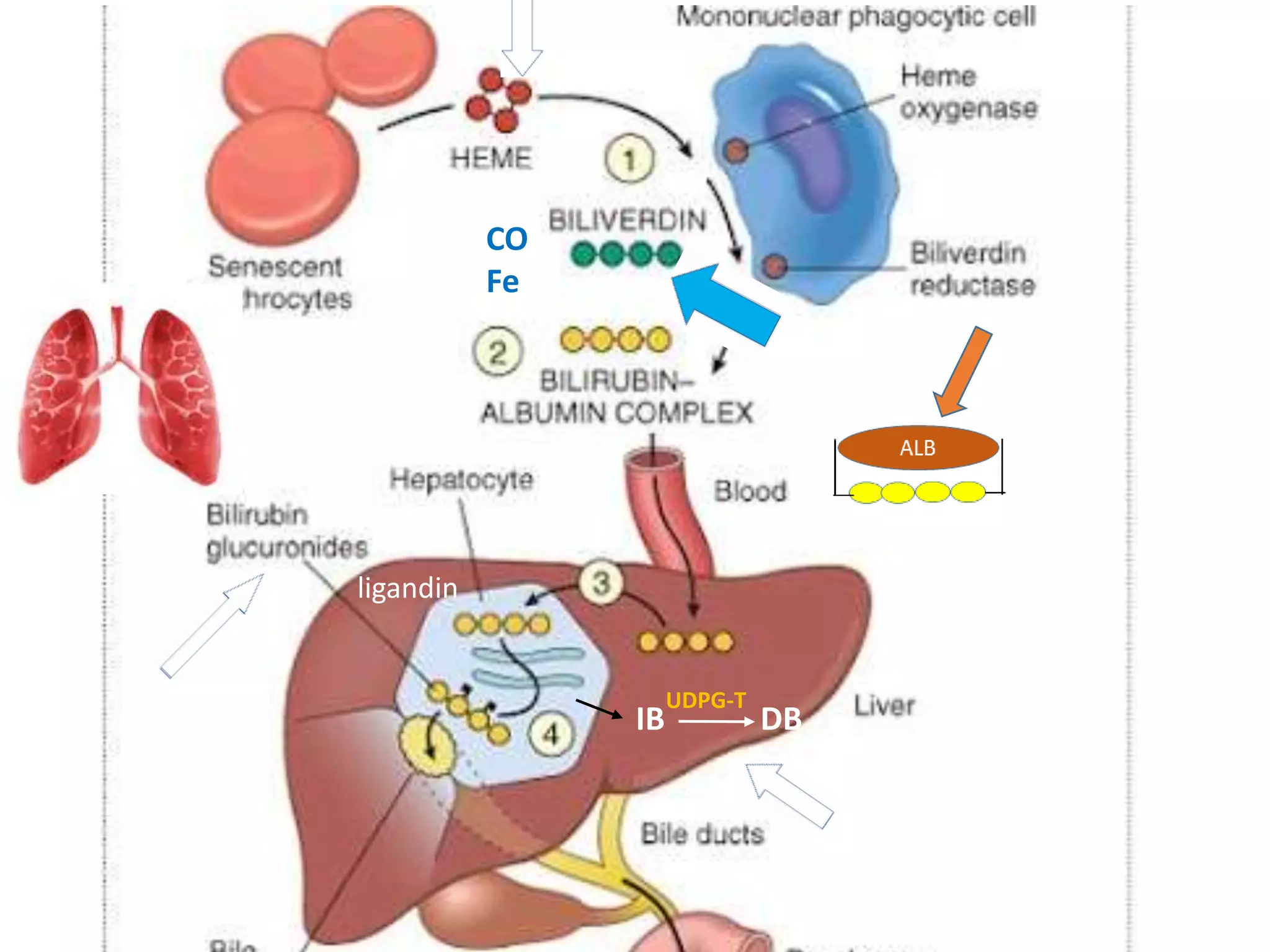
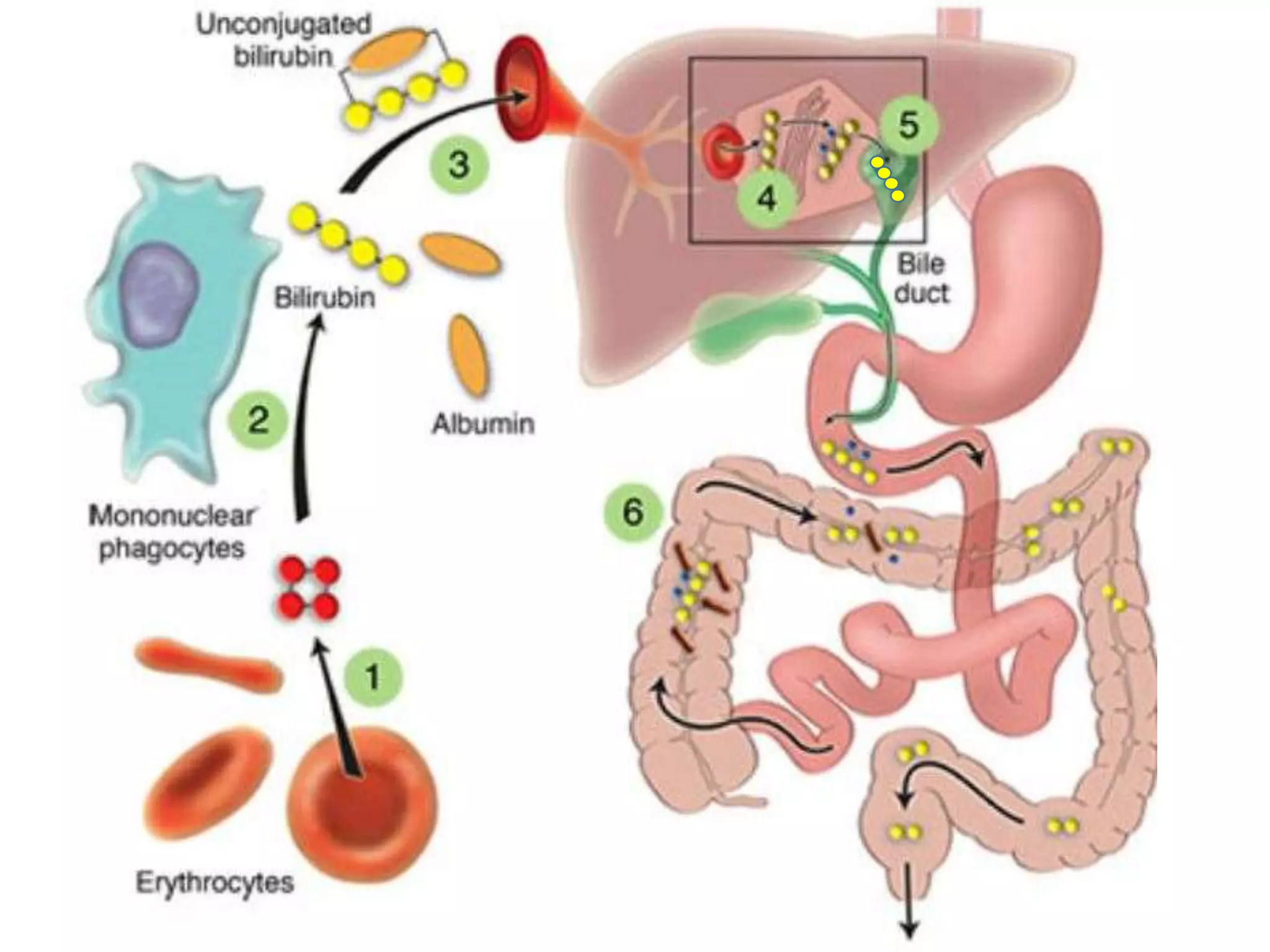
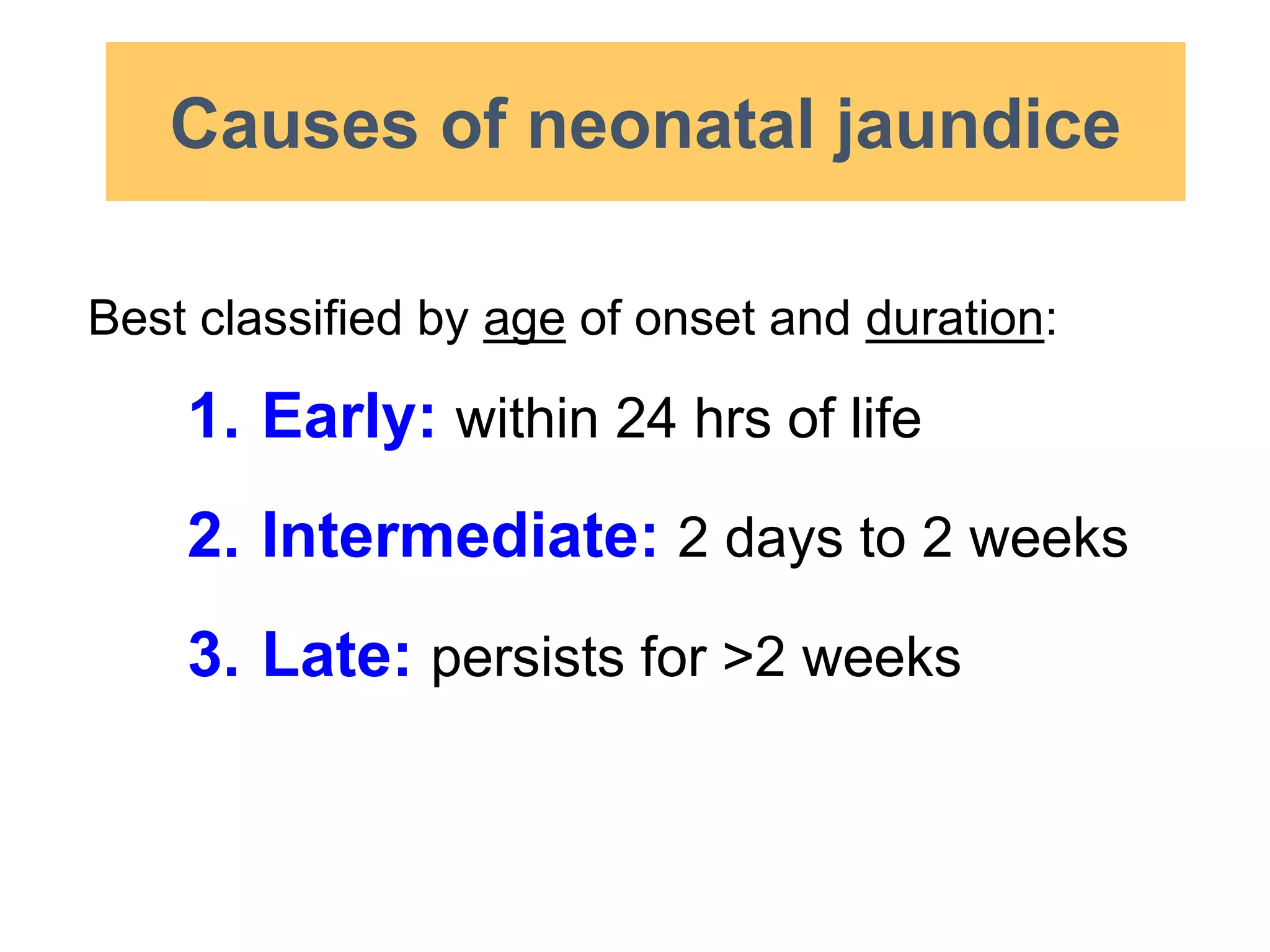
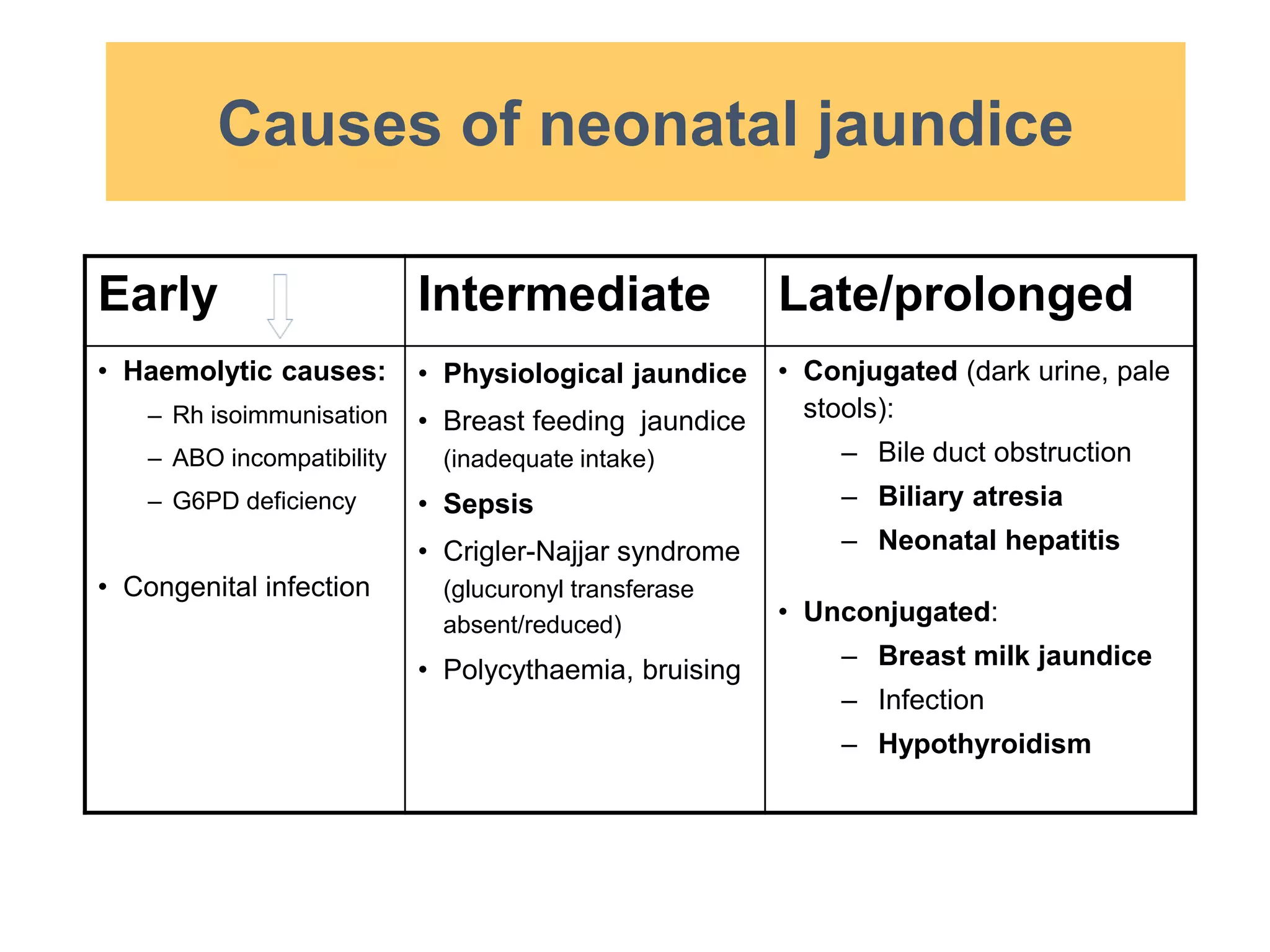
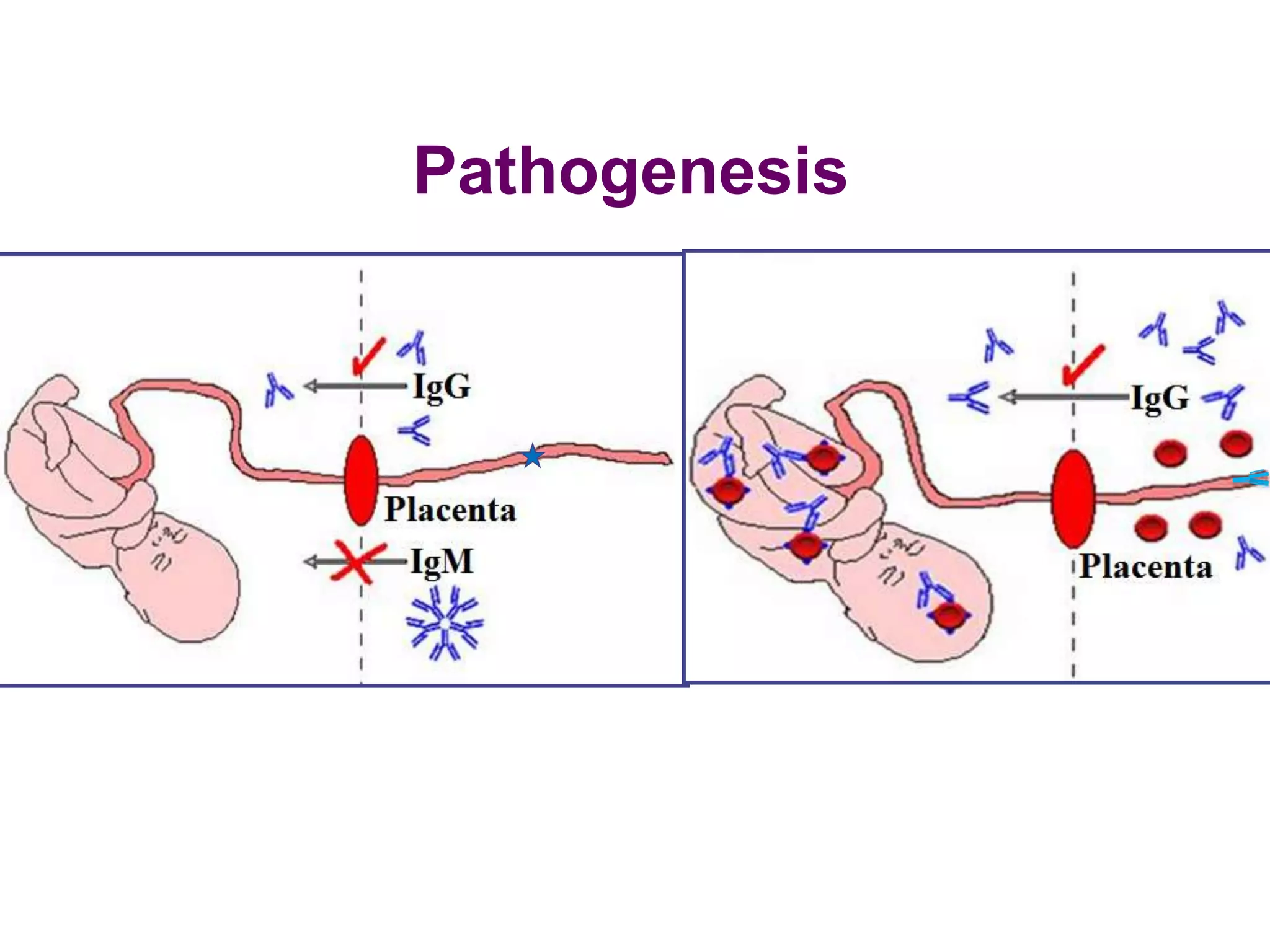
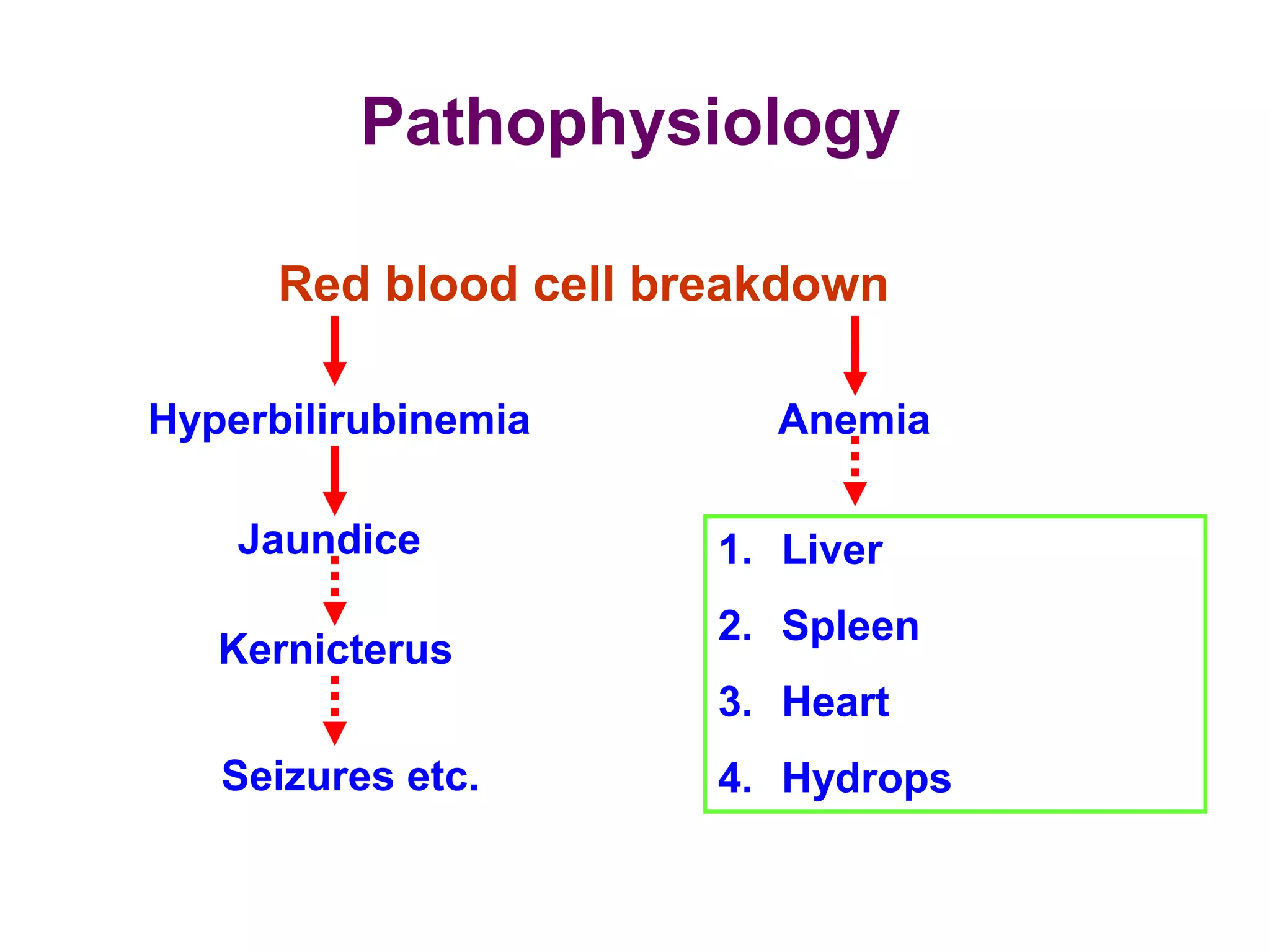
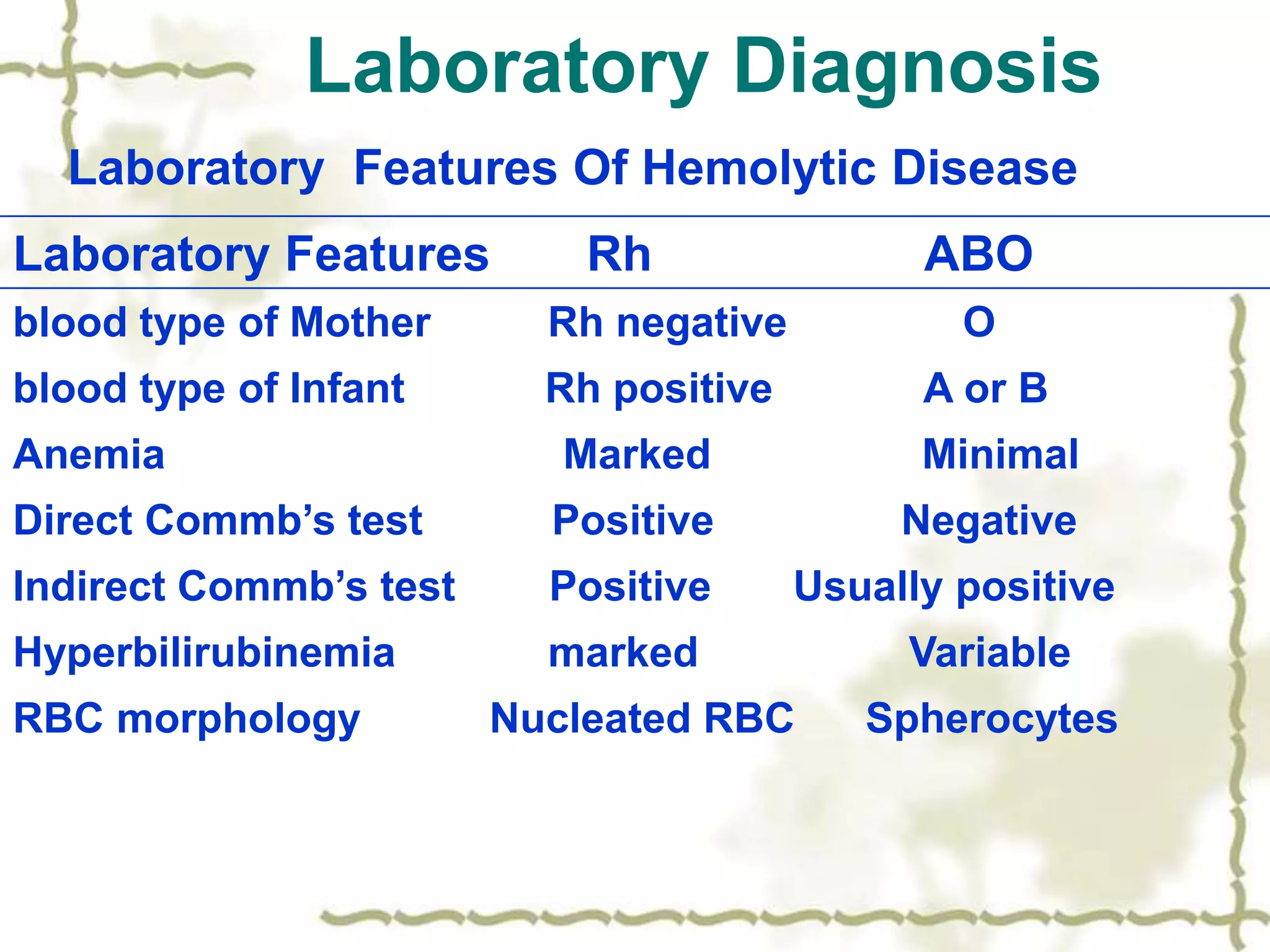
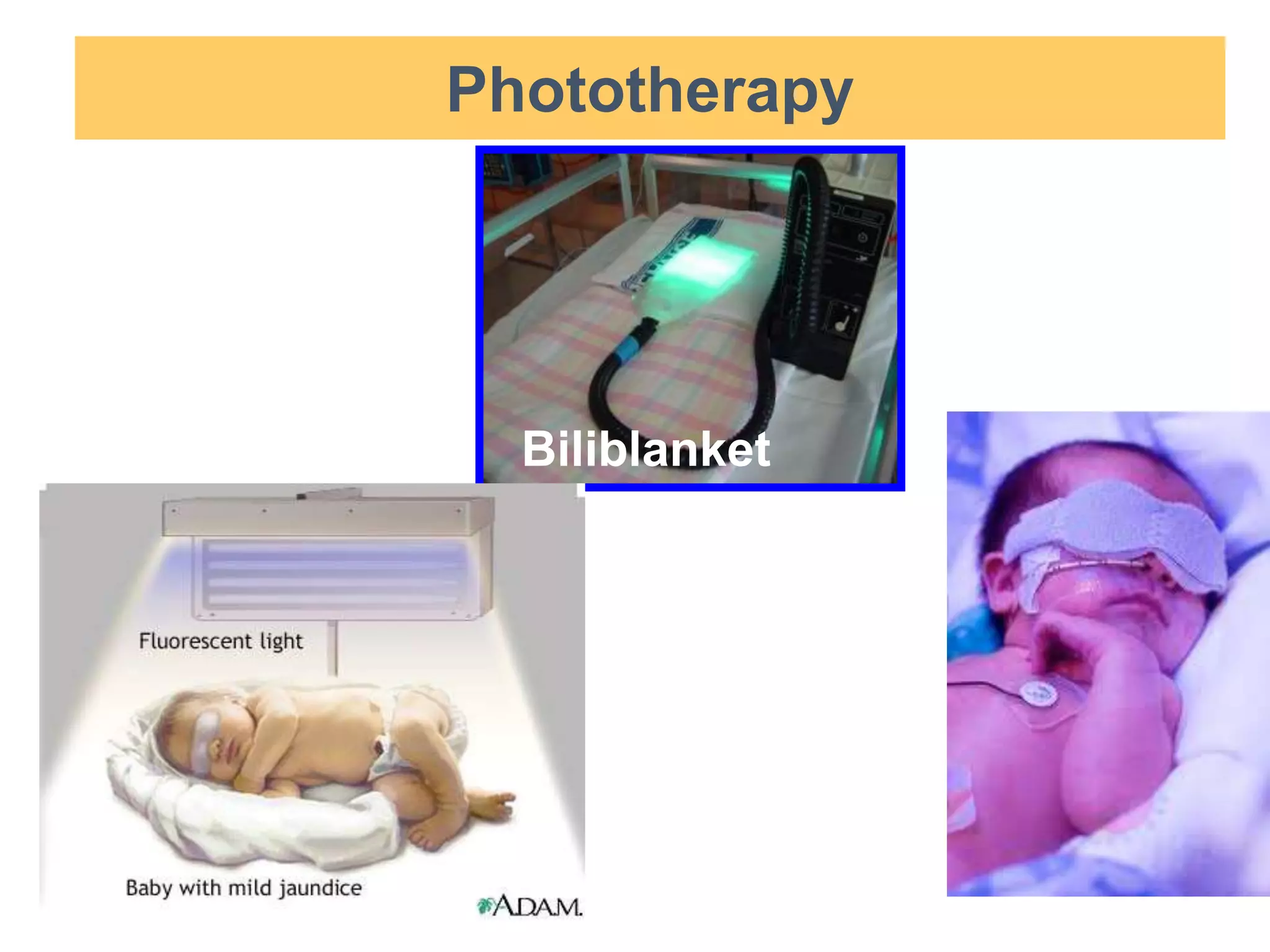
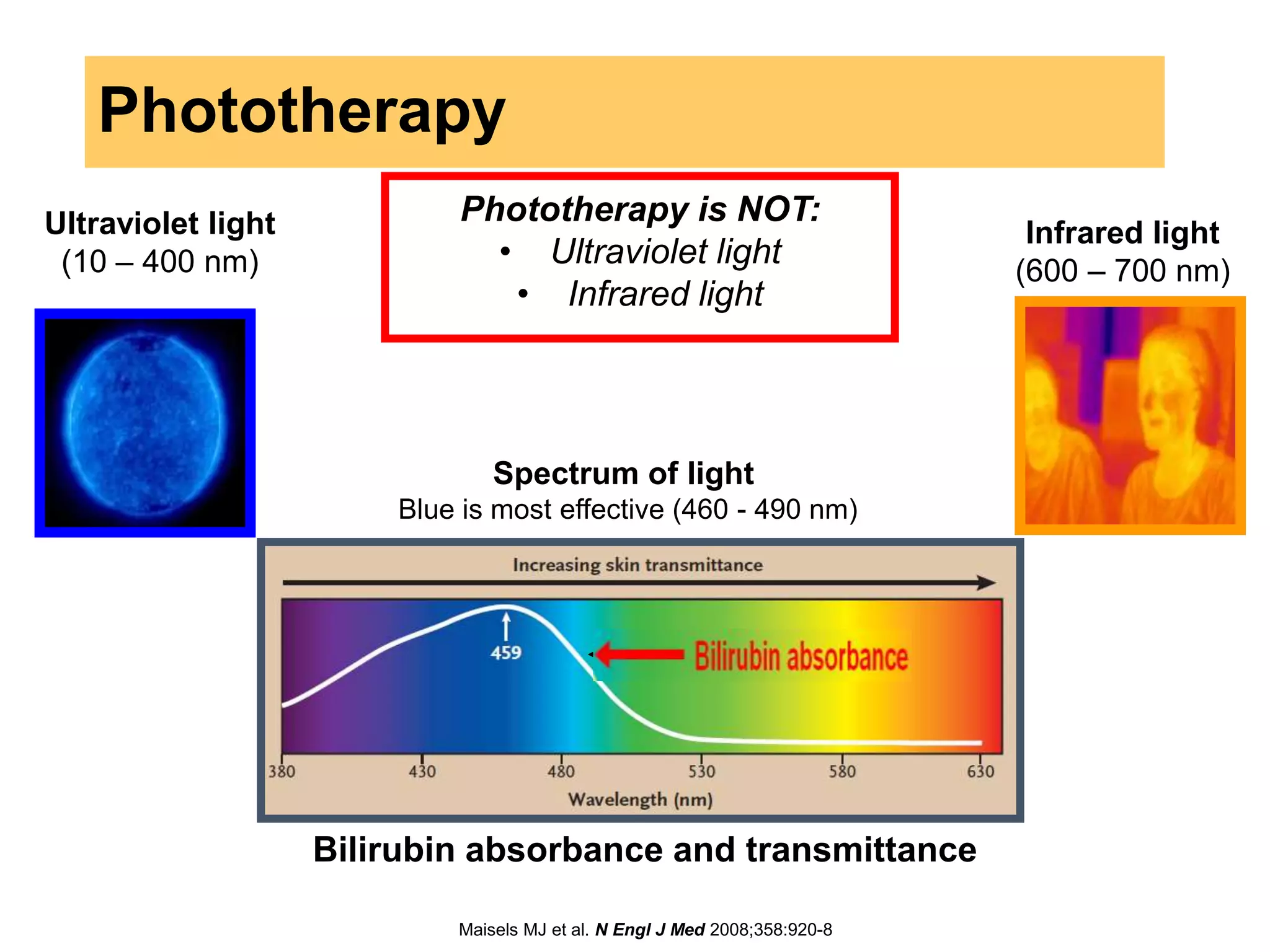
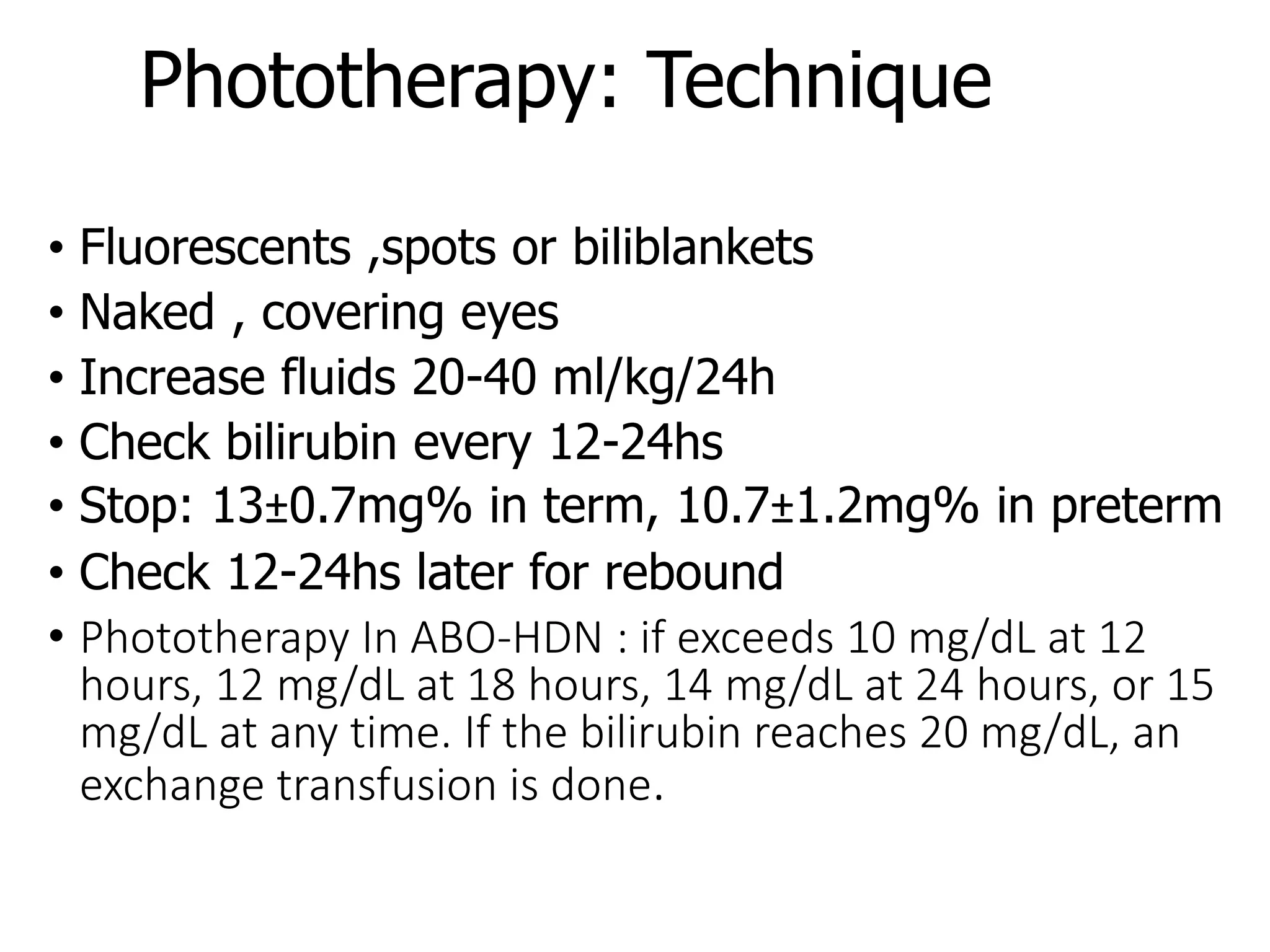
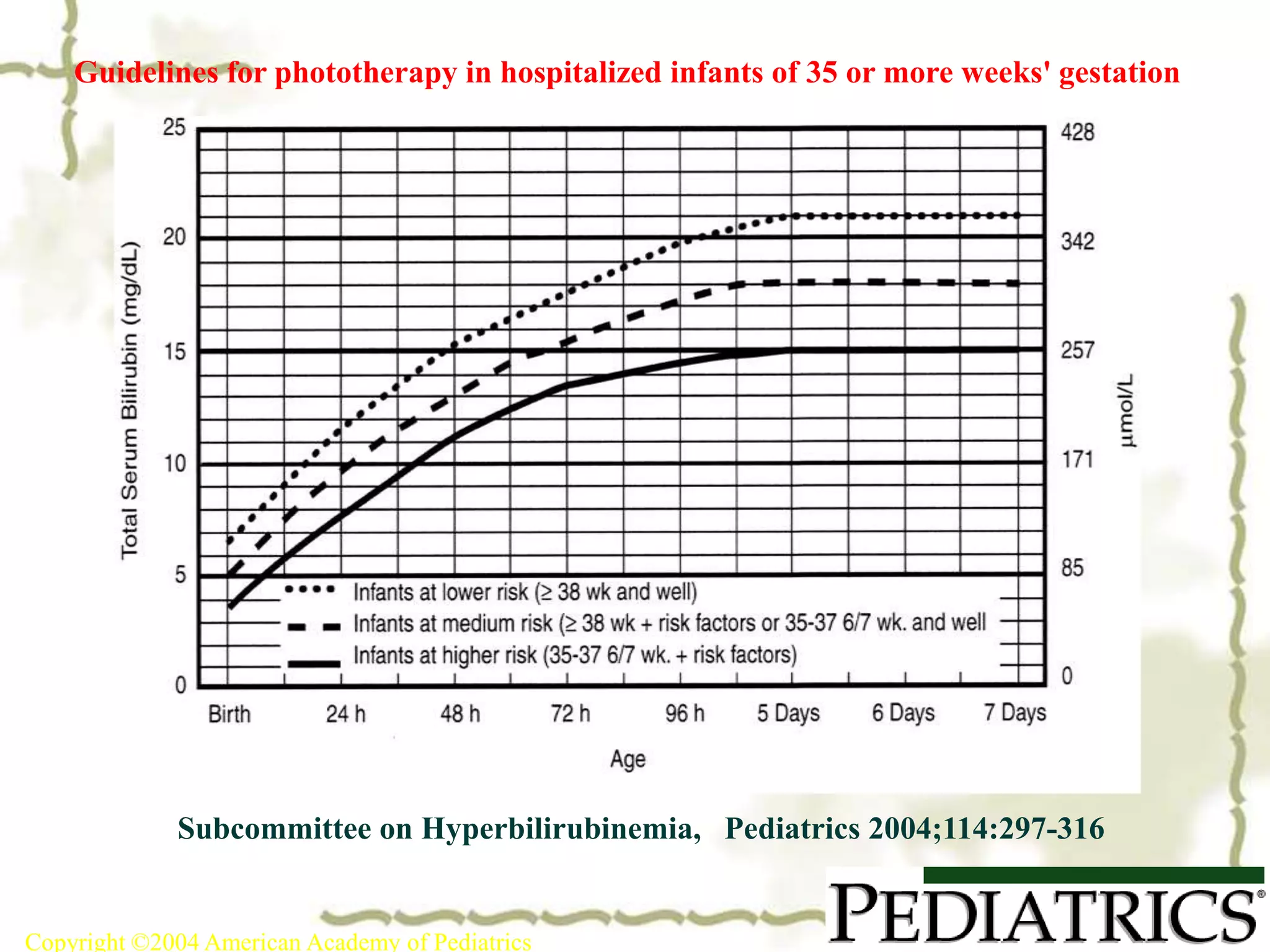
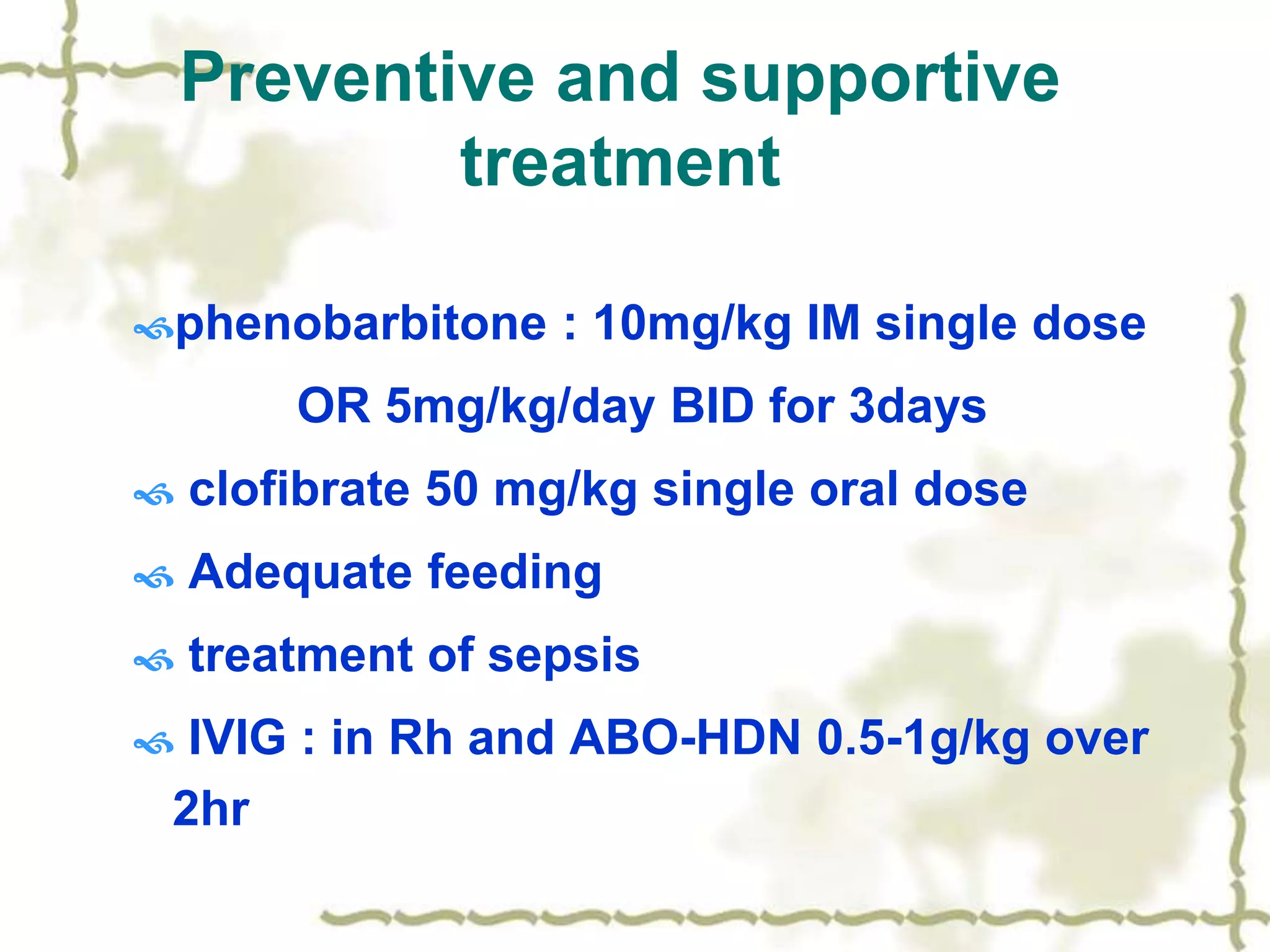
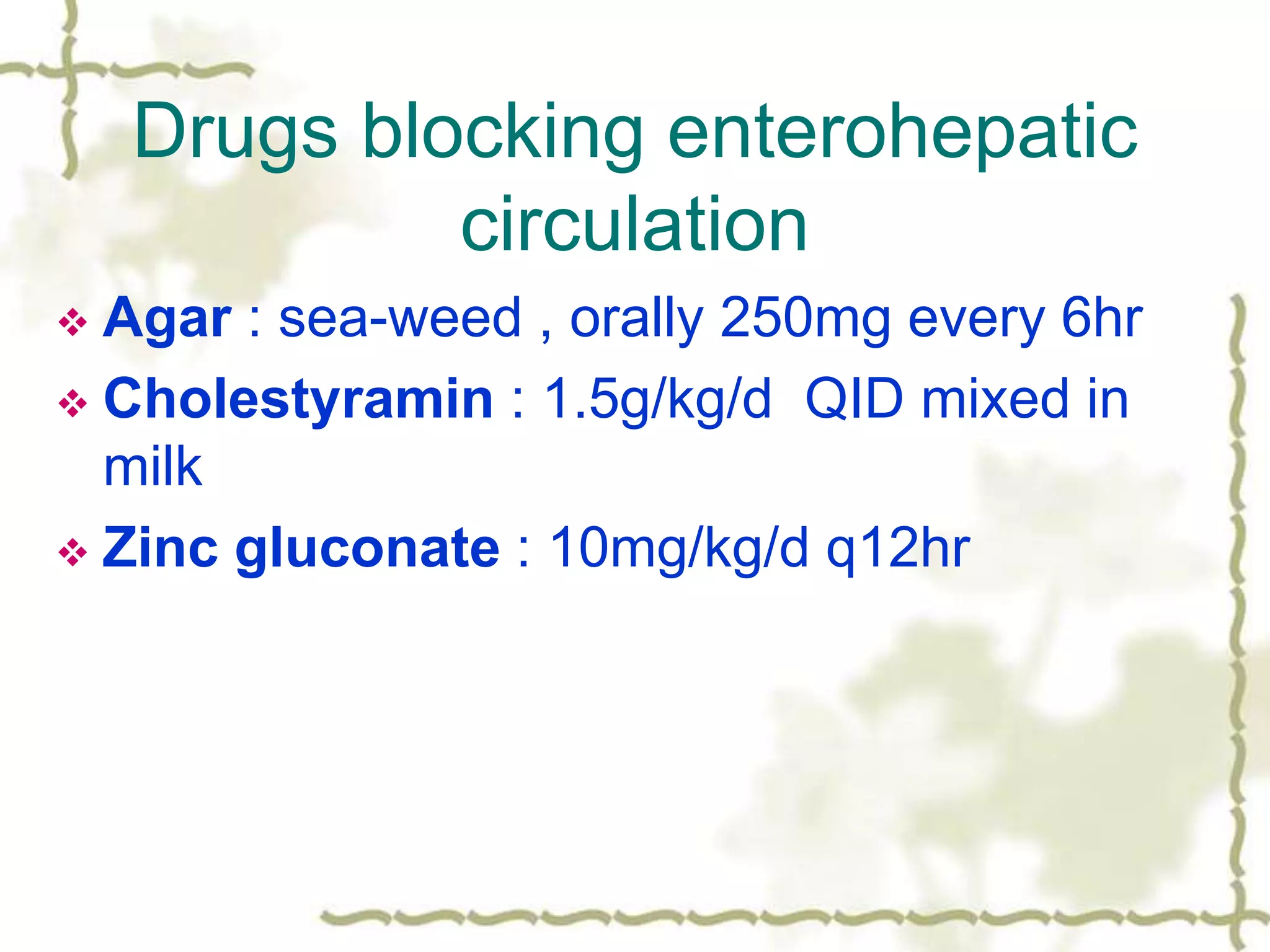
This document discusses ABO incompatibility, which is a type of hemolytic disease caused by a reaction between maternal anti-A or anti-B antibodies and fetal A or B antigens. It is usually milder than Rh incompatibility. The severity of hemolysis is greater in OA incompatibility. Treatment may include phototherapy or exchange transfusion if bilirubin levels are too high.