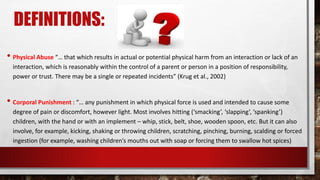
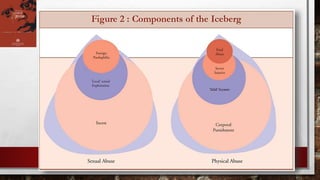
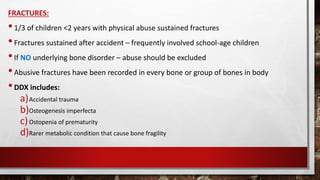
This document discusses child maltreatment in Malaysia. It provides definitions of different types of child abuse according to WHO, including physical abuse, sexual abuse, emotional abuse, neglect, and exploitation. It then summarizes prevalence rates of different types of abuse in several Southeast Asian countries based on various studies. The document also discusses risk factors for child abuse, signs that should raise suspicion of maltreatment, diagnostic approaches, and features that indicate abusive head trauma versus accidental head injuries in children.