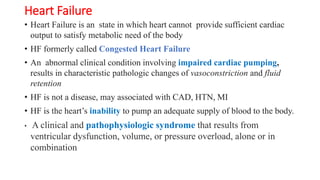
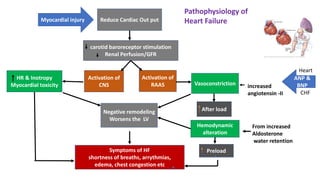
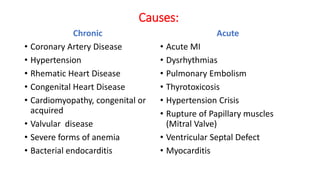
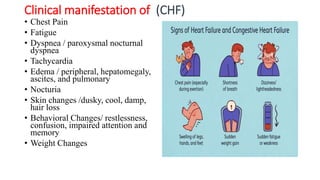
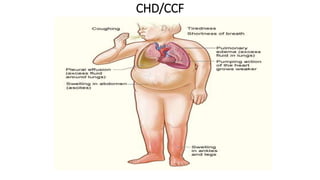
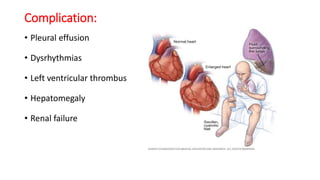
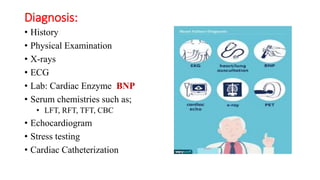
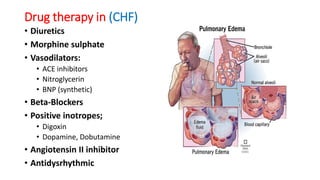
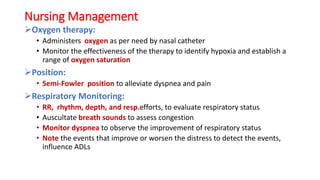
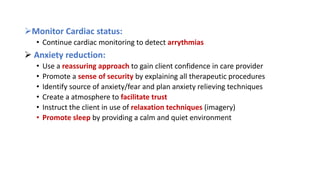
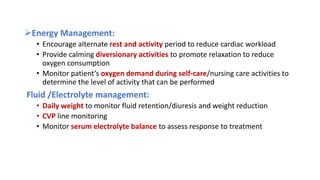
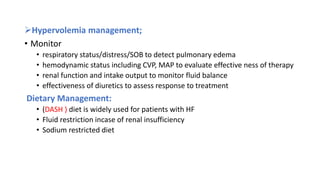
Heart failure occurs when the heart cannot pump enough blood to meet the body's needs. It can be caused by conditions that damage the heart such as coronary artery disease or hypertension. Symptoms include shortness of breath, fatigue, and edema. Treatment focuses on managing the underlying cause, restricting sodium and fluid intake, using diuretics and other drugs to reduce preload and afterload on the heart, and treating complications. Nursing care involves monitoring the patient's cardiac, respiratory and fluid status; managing anxiety and energy levels; and providing education on diet, medication, and lifestyle changes.