1. A 44-year-old man presented to the emergency room with chest pain, shortness of breath, palpitations, and nausea. His ECG showed ST elevation.
2. ST elevation myocardial infarction (STEMI) occurs when a coronary artery becomes blocked, cutting off blood supply and oxygen to the heart. The resulting cell death in the heart muscle is known as a heart attack.
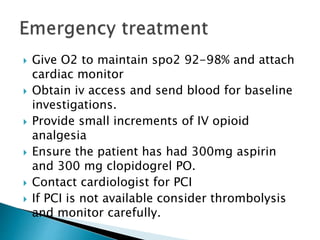
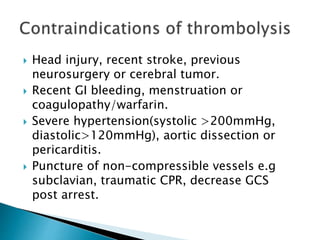
3. Given his symptoms and ECG findings, the next step in his management should be to administer aspirin and clopidogrel, provide oxygen, monitor him closely, and contact a cardiologist for urgent percutaneous coronary intervention (PCI) to reopen the blocked artery if possible within 90 minutes. If PCI is