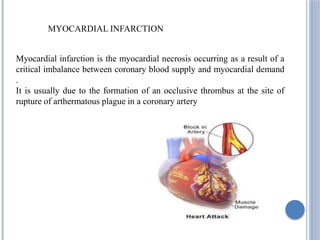
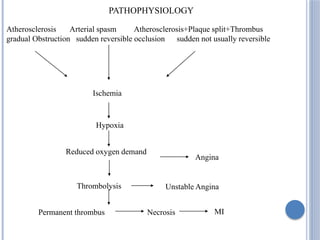
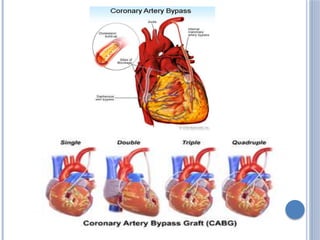
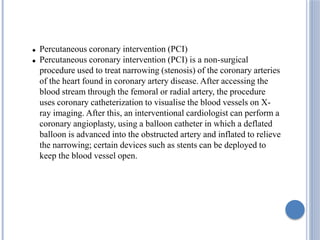
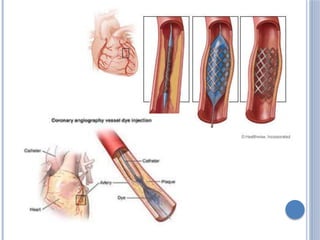
This document defines myocardial infarction and describes its types, causes, symptoms, complications, diagnostic tests, and treatment options. Myocardial infarction is the death of heart muscle caused by a blockage in one of the coronary arteries that reduces blood flow. It can be anterior, posterior, or other regions. Risk factors include smoking, hypertension, age, and diabetes. Symptoms include chest pain and shortness of breath. Complications include heart failure, arrhythmias, and cardiac rupture. Diagnosis involves electrocardiograms, blood tests of cardiac enzymes, and imaging tests. Treatment includes medications like aspirin, beta-blockers, and statins as well as surgical procedures like coronary artery bypass grafting and angioplasty