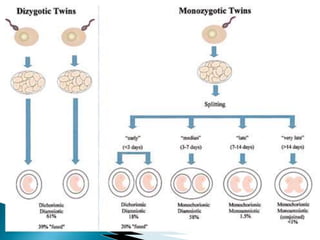
This document defines types of multiple pregnancies from twins to septuplets and provides information on the incidence, causes, development, and risks of twin pregnancies. It discusses monozygotic and dizygotic twins, their genetic differences, and the various types of conjoined twins. Risks of twin pregnancies include preeclampsia, anemia, preterm birth, and increased operative delivery. Ultrasound is used to determine chorionicity and monitor growth. Close antenatal monitoring and skilled delivery are important due to risks of complications.