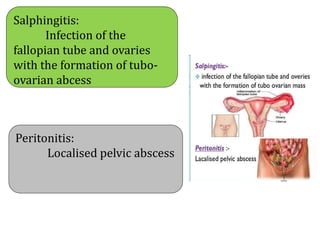
This document defines puerperal infection and discusses its causes, risk factors, modes of infection, pathophysiology, clinical features, diagnosis, prevention and treatment. Puerperal infection is defined as an infection developing in the birth structures after delivery. It is caused by bacteria entering through the genital tract during or after delivery. Risk factors include malnutrition, anemia, prolonged rupture of membranes, and traumatic deliveries. Symptoms range from mild fever to sepsis. Diagnosis involves cultures of blood, urine and vaginal swabs. Treatment consists of antibiotics, drainage of abscesses, and sometimes hysterectomy for severe cases. Prevention focuses on identifying and managing risk factors during prenatal and intranatal care.