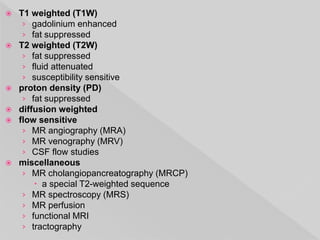
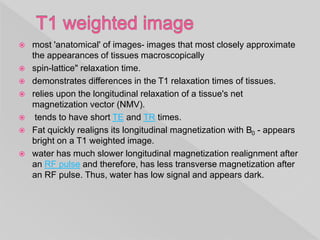
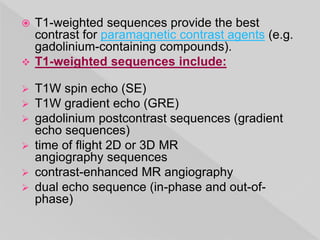
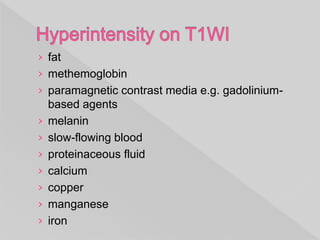
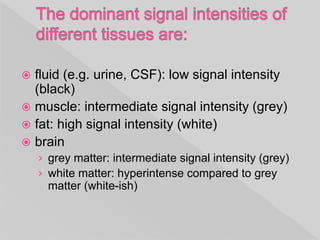
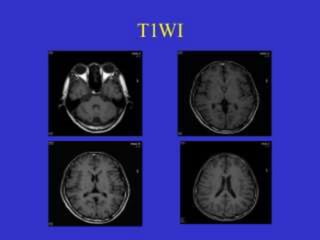
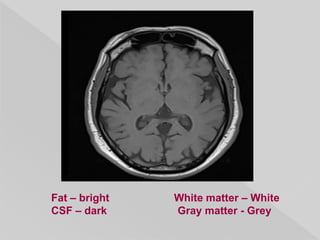
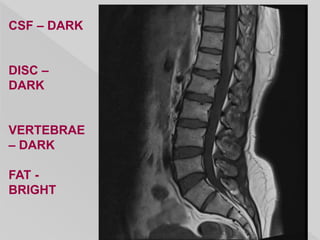
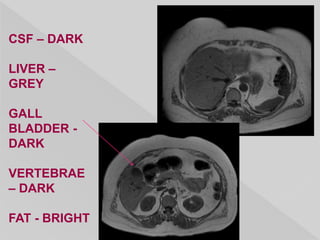
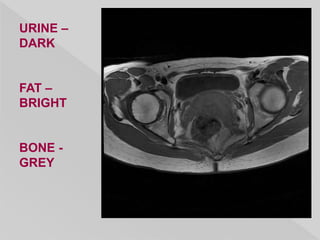
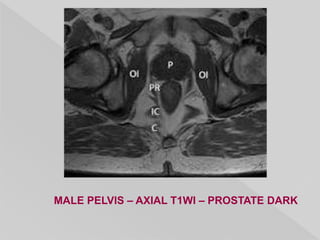
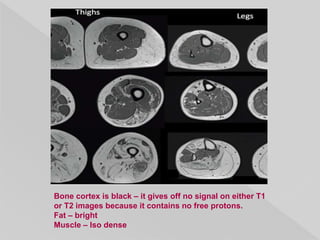
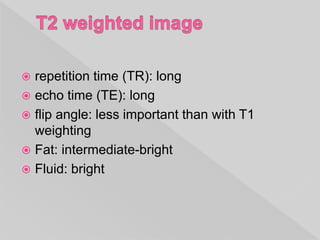
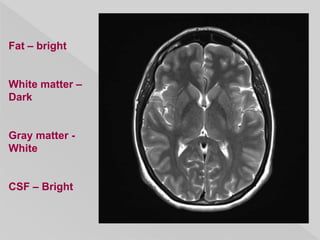
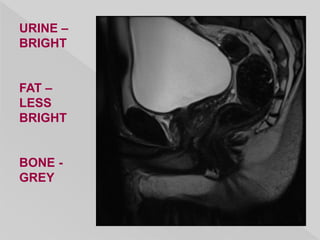
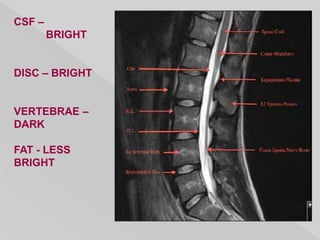
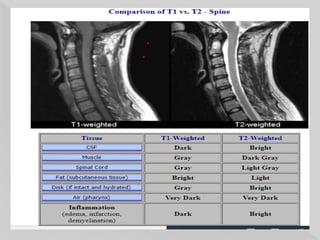
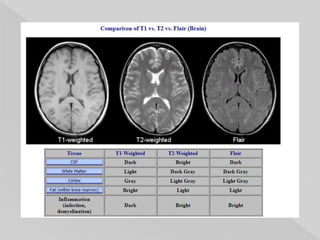
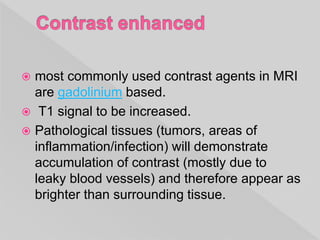
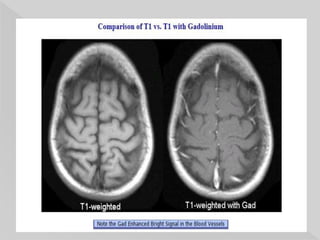
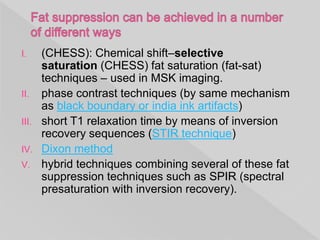
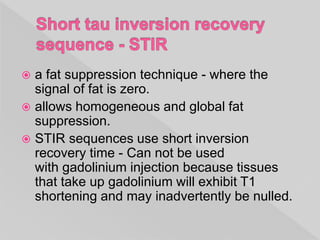
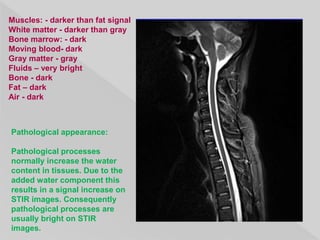
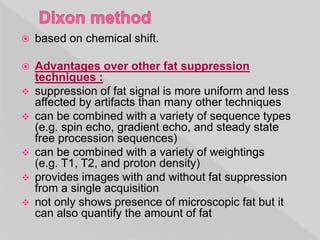
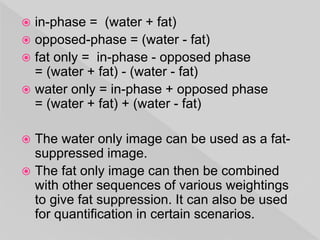
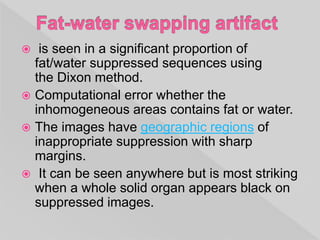
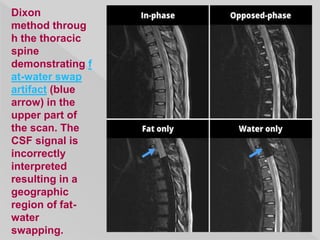
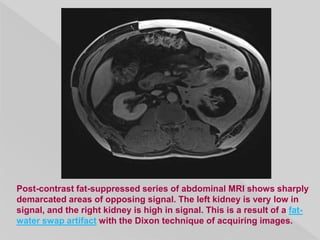
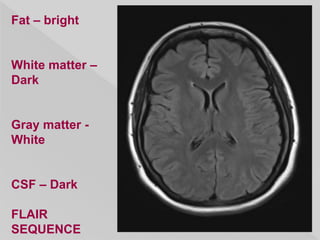
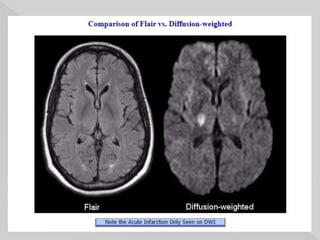
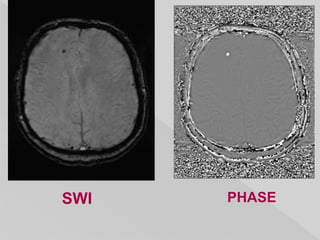
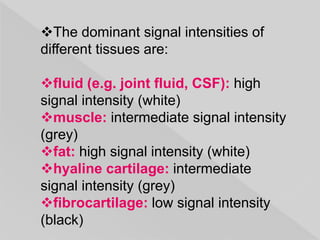
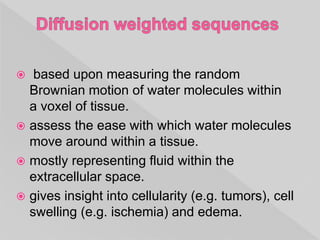
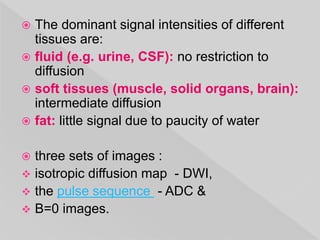
This document provides information on different MRI sequences and their characteristics. It discusses T1-weighted, T2-weighted, proton density, diffusion weighted, flow sensitive, and miscellaneous sequences such as MRCP, MRS, perfusion and tractography. Specific tissues and their appearance on different sequences are described. Techniques for fat suppression and their advantages are also outlined.