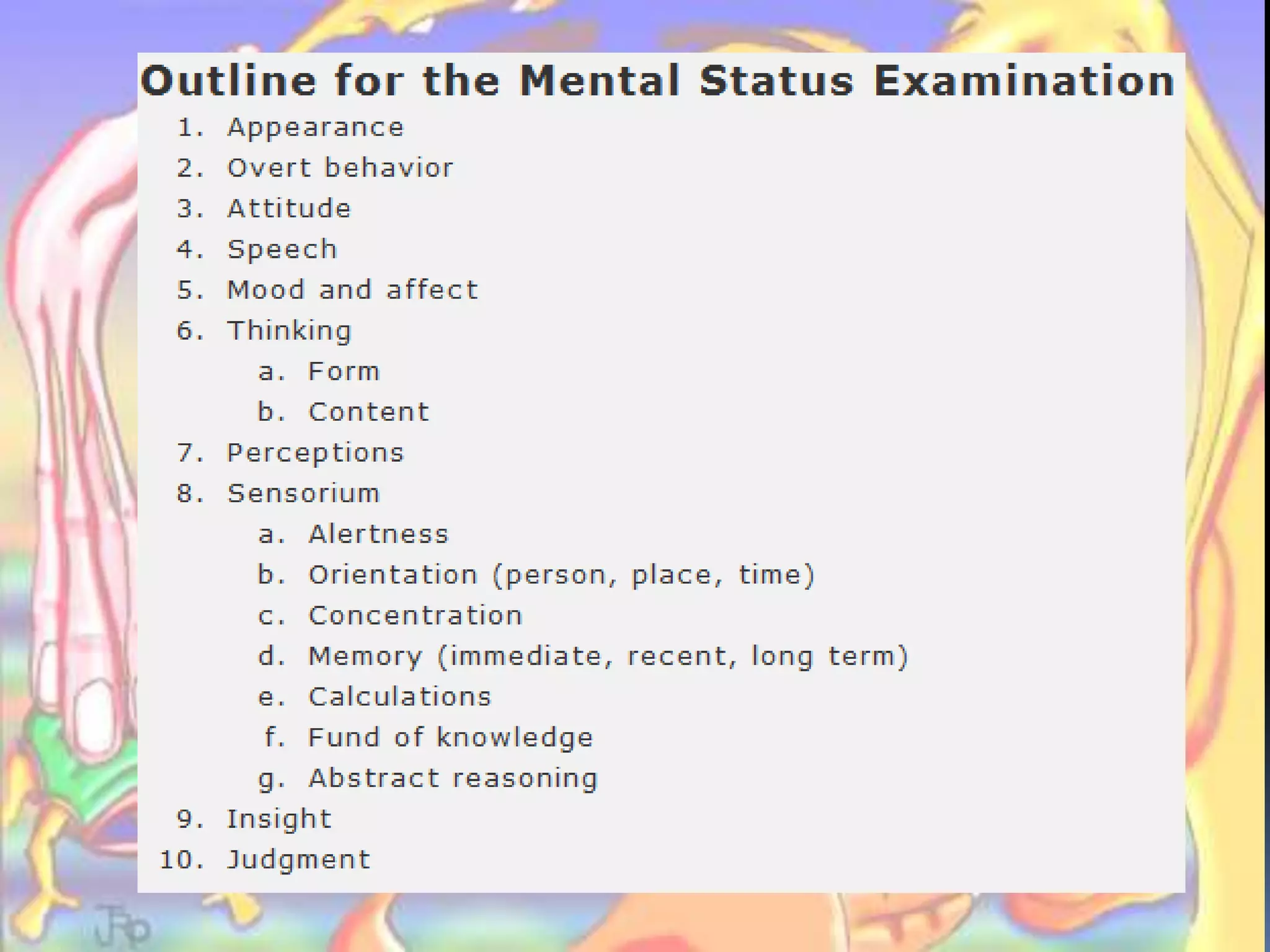
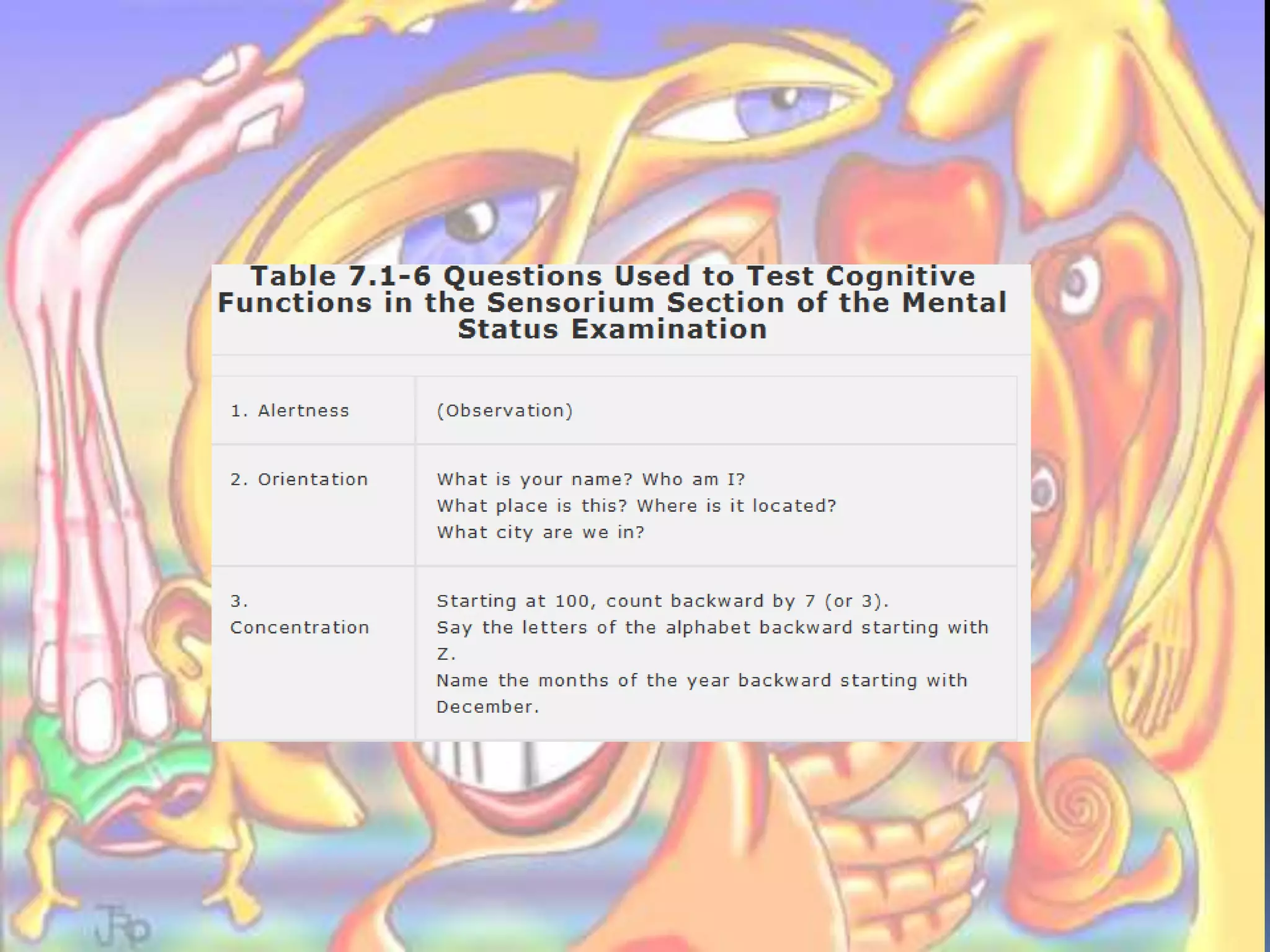
This document describes the components of a mental status examination used to evaluate psychiatric patients. It involves assessing a patient's appearance, speech, behavior, mood, thought processes, memory, orientation, judgment, insight and other cognitive functions. The exam is used to describe the patient's condition at the time of interview and obtain an overall impression of their mental health status.