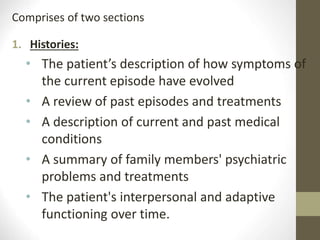
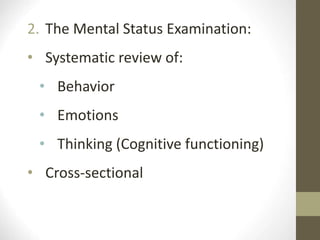
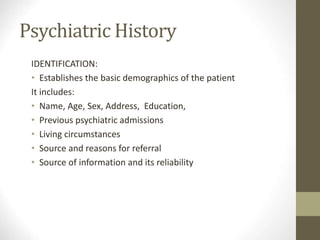
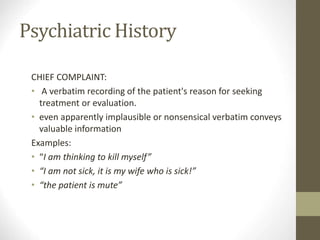
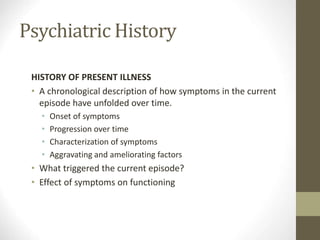
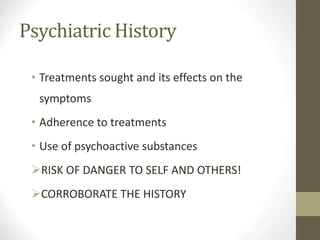
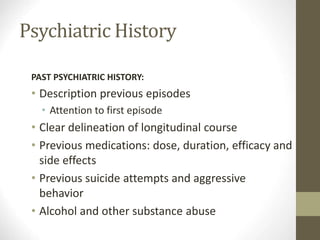
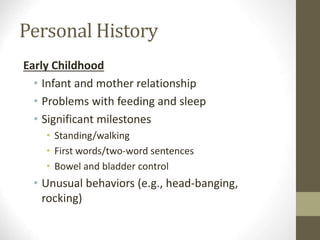
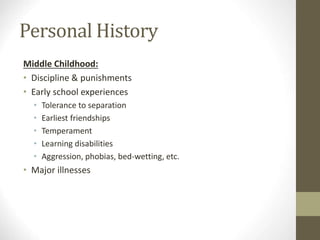
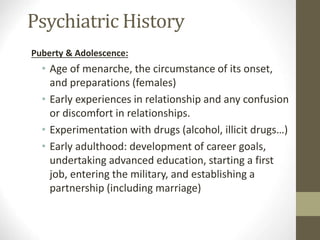
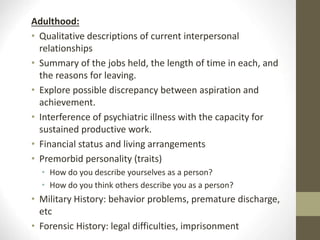
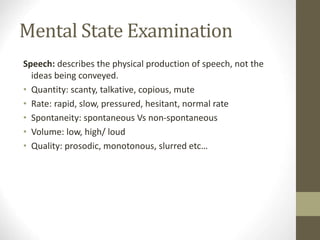
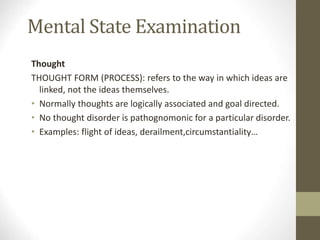
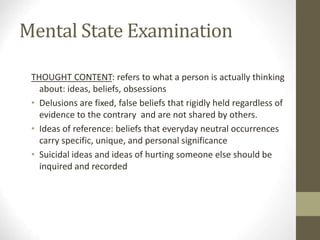
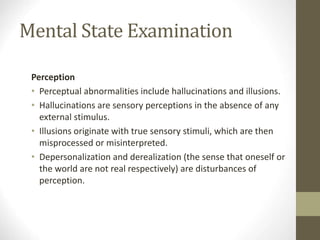
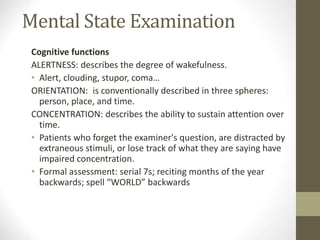
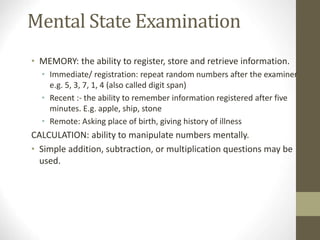
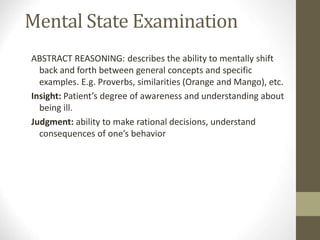
The document describes the components of a psychiatric evaluation, which includes a psychiatric history and mental status examination. The psychiatric history comprises histories of the present illness, past psychiatric and medical history, family history, and personal history. The mental status examination involves assessing appearance, behavior, mood, thought processes, cognition, and perception. Together these components provide essential information about a patient's condition and history to inform diagnosis and treatment.