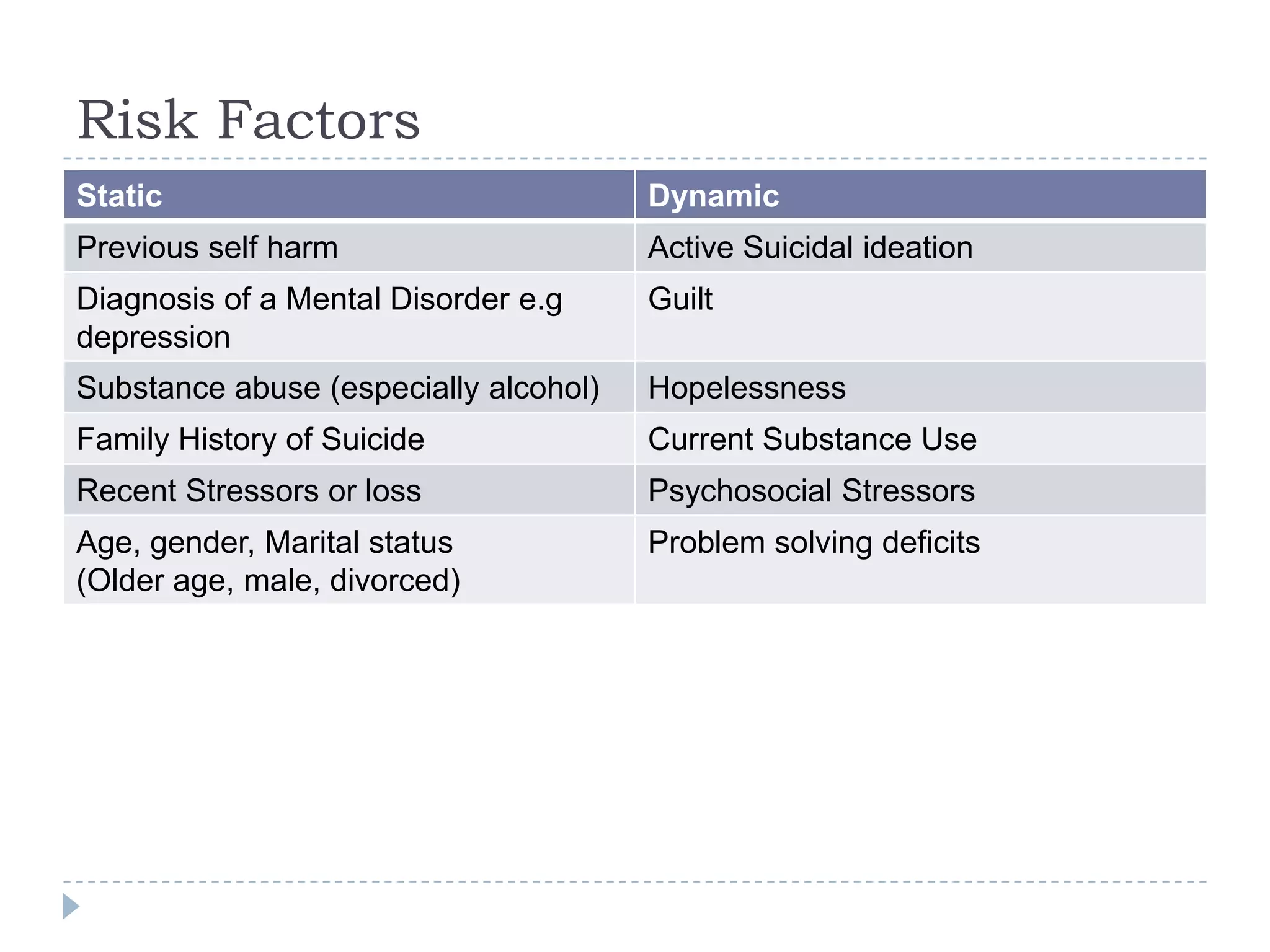
This document discusses mental health risk assessment and management. It notes that clinicians have poor ability to predict suicide or homicide. It identifies static risk factors like previous self-harm and dynamic factors like suicidal ideation. Guidelines are provided for asking patients about suicidal thoughts and developing safety plans. Involuntary referral criteria and processes are outlined when significant short-term risk is present.








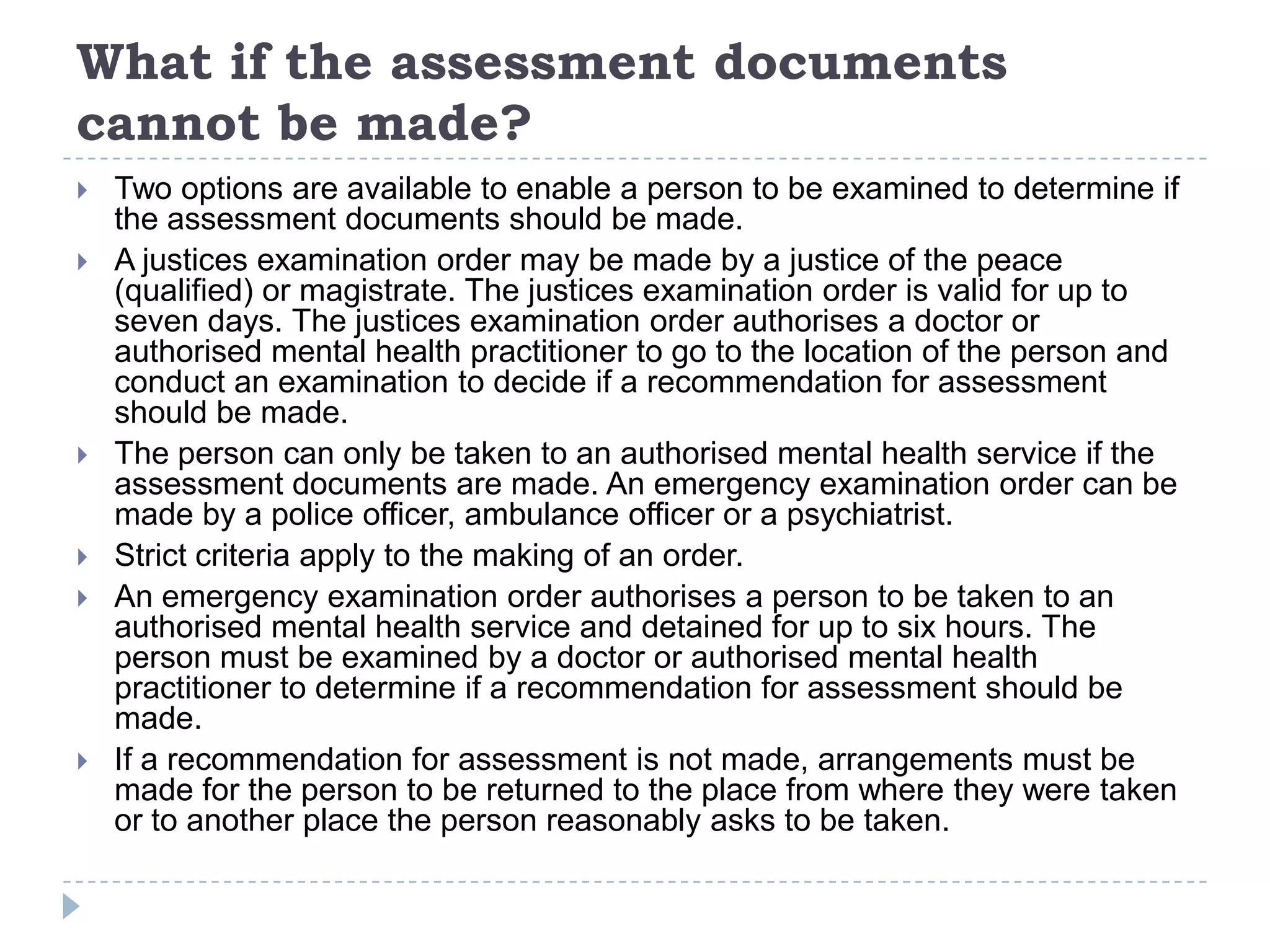

![Section 13
What are the assessment criteria
(1) The assessment criteria for a person, are all of the
following, based on available information
(a) the person appears to have a mental illness;
(b) the person requires immediate assessment;
(c) the assessment can properly be made at an authorised mental
health service;
(d) there is a risk that the person may—
(i) cause harm to himself or herself or someone else;
or
(ii) suffer serious mental or physical deterioration;
(e) there is no less restrictive way of ensuring the person is
assessed.
(2) Also, for chapter 2, the assessment criteria for a person
include
(a) lacking the capacity to consent to be assessed; or
(b) having unreasonably refused to be assessed.[s 14]](https://image.slidesharecdn.com/mentalhealthriskassessment-13381045367978-phpapp02-120527024405-phpapp02/75/Mental-Health-Risk-Assessment-14-2048.jpg)