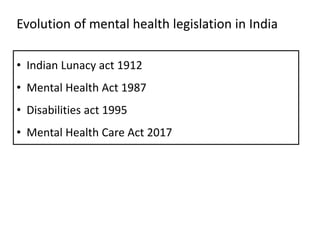
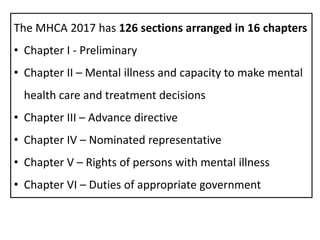
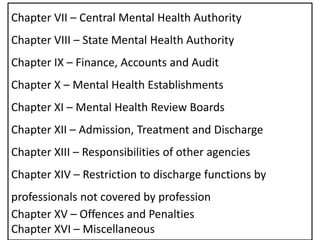
The document summarizes the Mental Health Care Act of 2017 in India. Some key points:
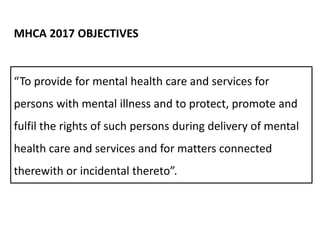
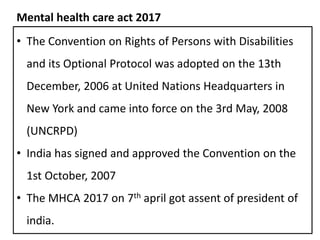
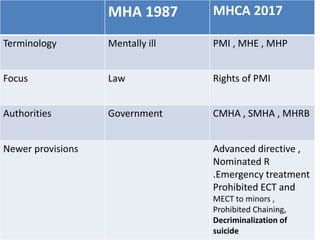
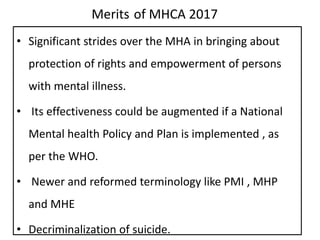
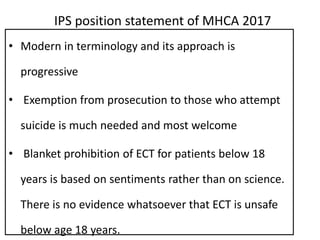
- The Act was passed in 2017 to provide legal framework for mental healthcare and protect rights of those with mental illness.
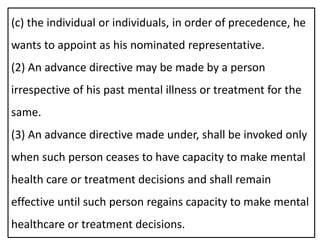
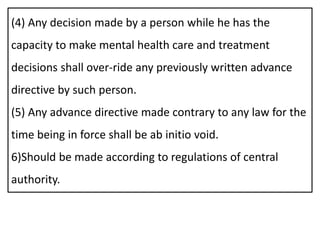
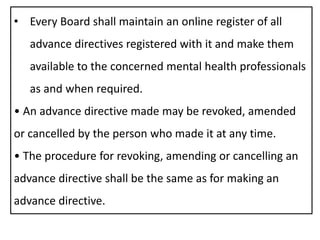
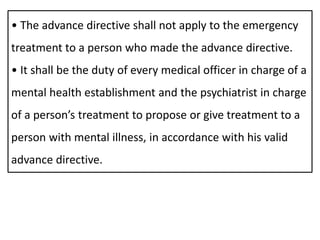
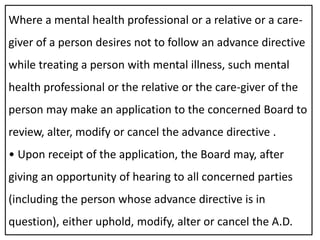
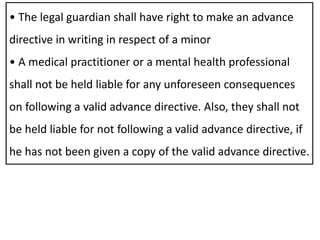
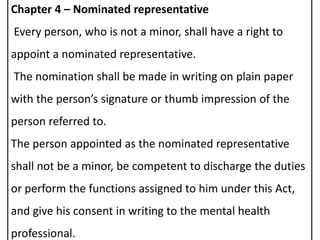
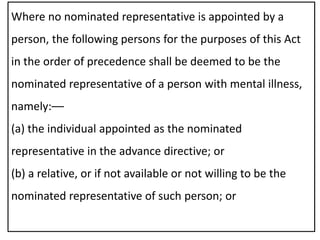
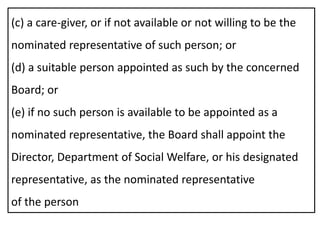
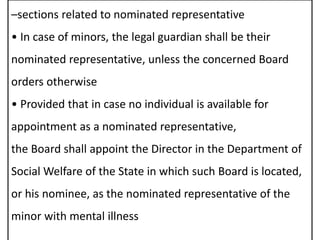
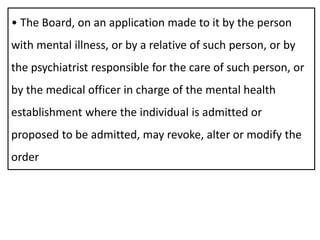
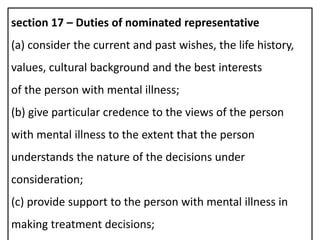
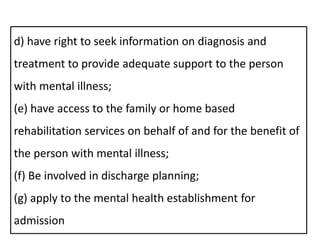
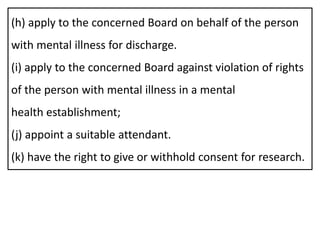
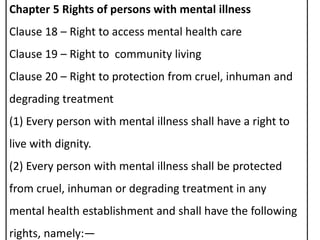
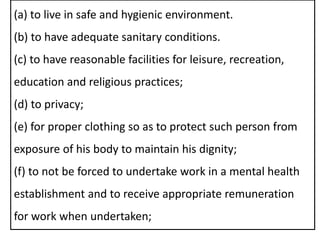
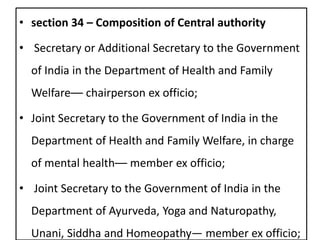
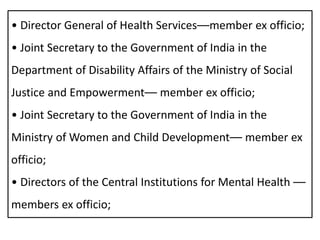
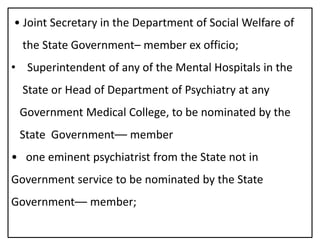
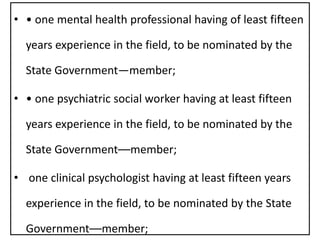
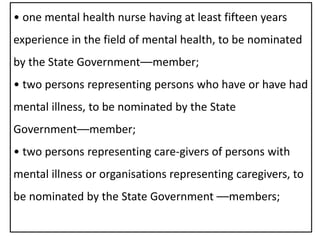
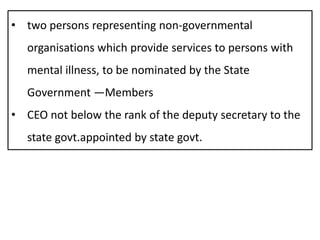
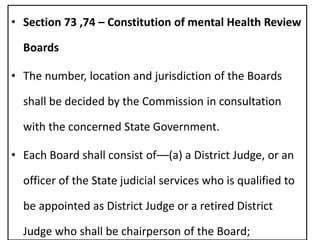
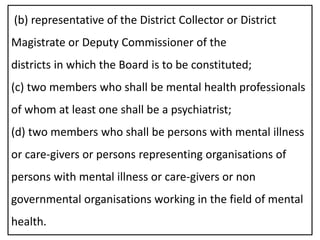
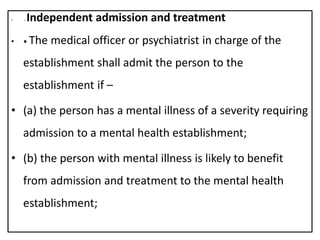
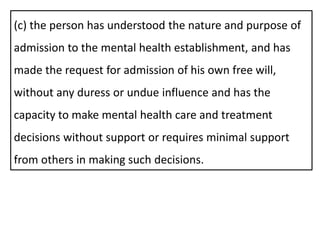
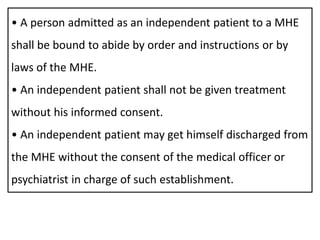
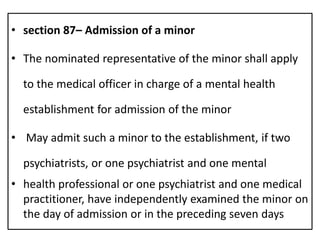
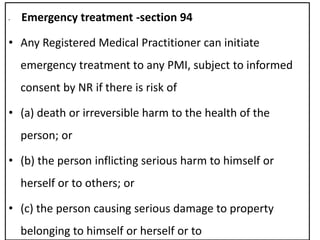
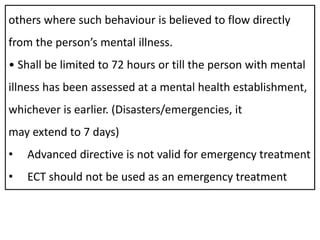
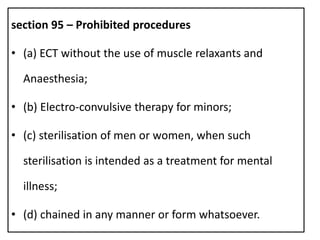
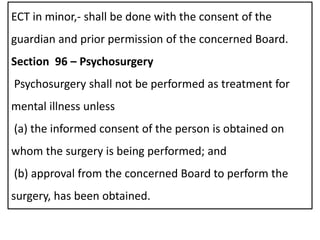
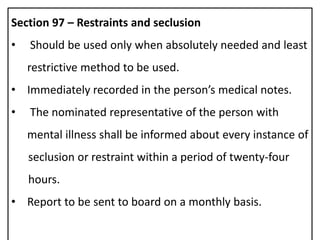
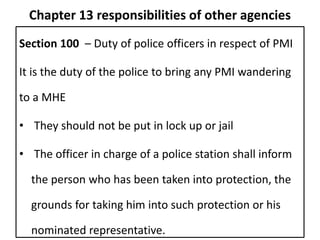
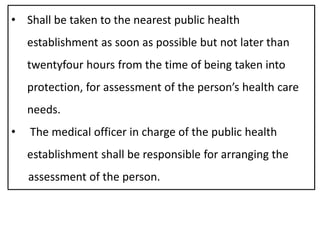
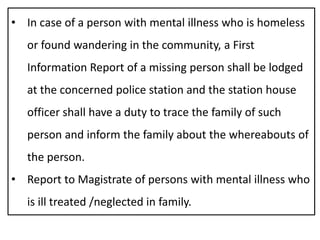
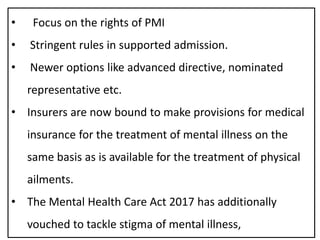
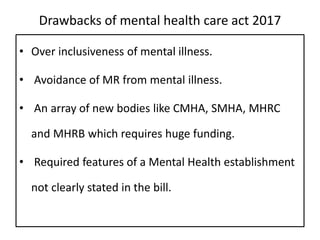
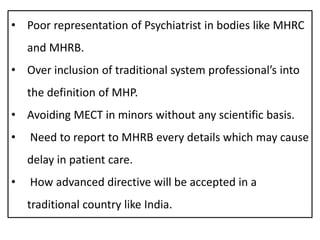
- It outlines provisions for advance directives, nominated representatives, rights of those with mental illness, and establishment of central and state mental health authorities.
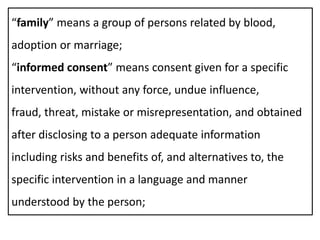
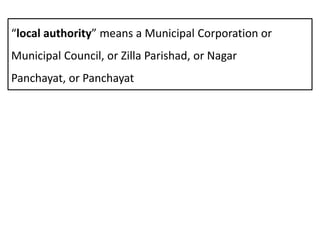
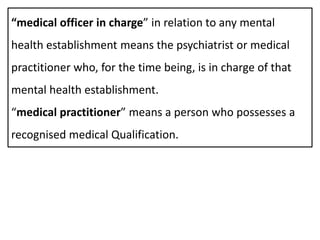
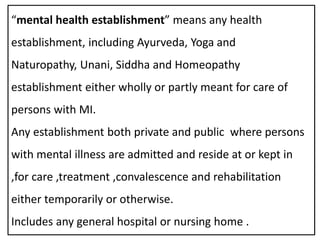
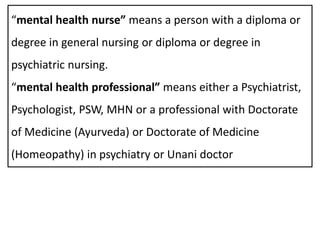
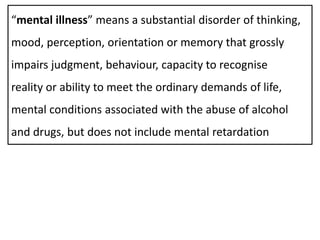
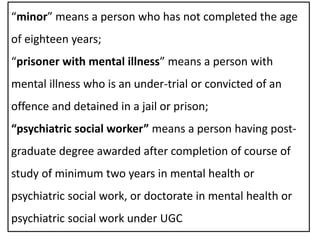
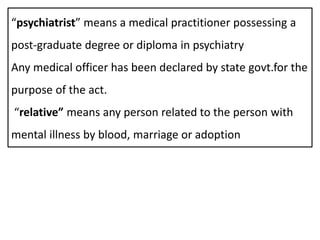
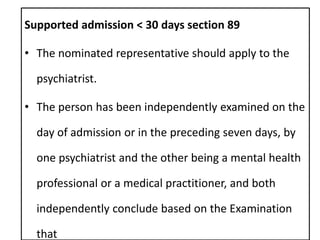
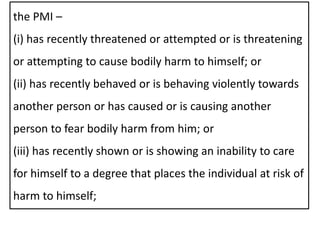
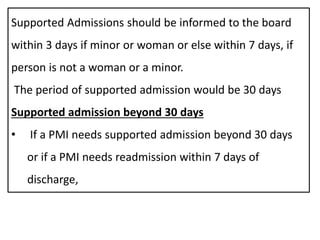
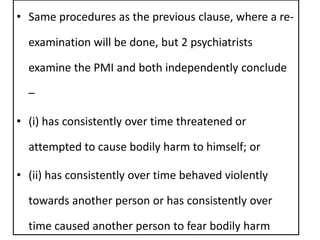
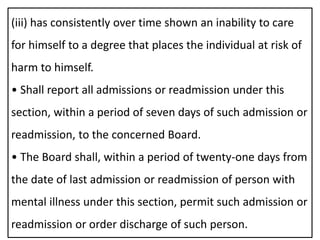
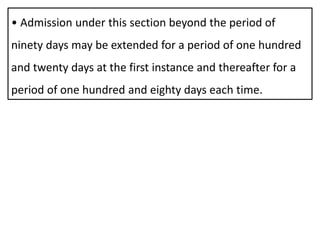
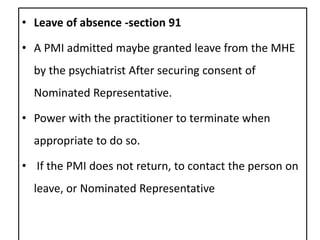
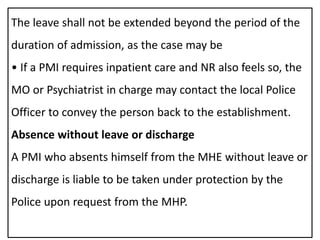
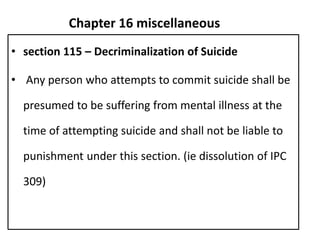
- The Act has 16 chapters covering definitions of key terms, determination of mental illness, consent procedures, admission/discharge processes, and offenses/penalties. It aims to improve community integration and access to high quality care for those suffering from mental illness.