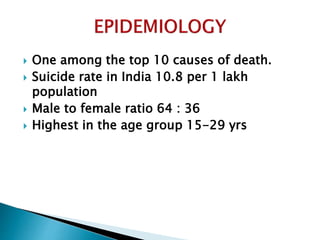
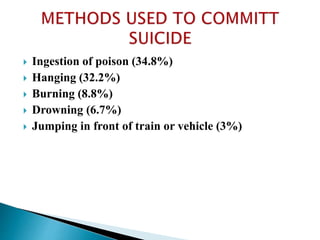
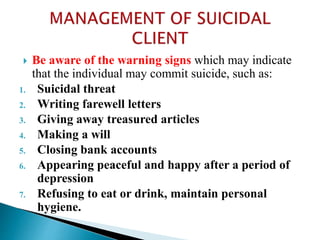
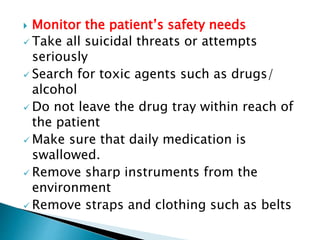
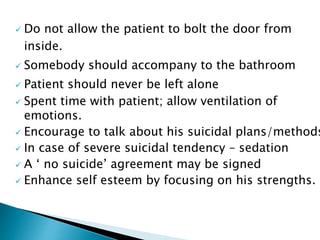
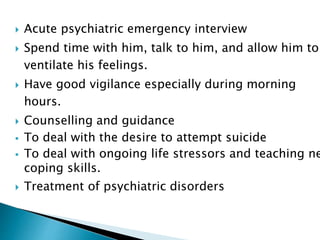
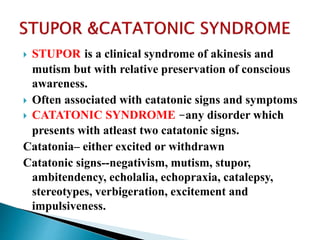
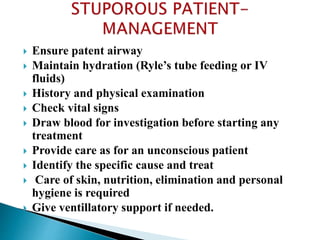
This document discusses various topics related to psychiatric emergencies. It defines psychiatric emergency as a condition wherein the patient has disturbances of thought, affect and psychomotor activity leading to a threat to their existence or others. It describes suicide, violence, stupor, crisis and bewilderment. It provides guidelines for handling psychiatric emergencies, focusing on initial approach, evaluation and care based on seriousness. Specific conditions discussed include suicide, violence, stupor and catatonic syndrome. It outlines assessment and management for each condition.

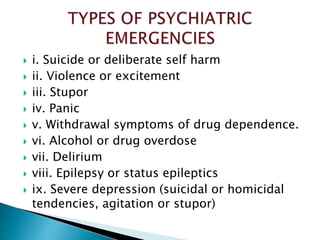



![ Following epileptic attack patient may behave in a
strange manner and become excited and violent.
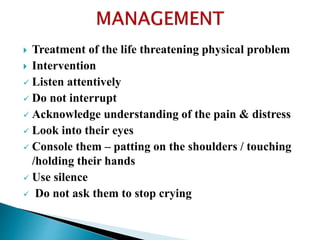
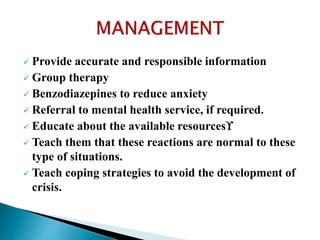
Management:
Sedation: Inj. Diazepam 10 mg IV [or] Inj. Luminal
10 mg IV followed by oral anticonvulsants.
Haloperidol 10 mg IV helps to reduce psychotic
behaviour.](https://image.slidesharecdn.com/psychiatricemergencies-200715110302/85/PSYCHIATRIC-EMERGENCIES-66-320.jpg)