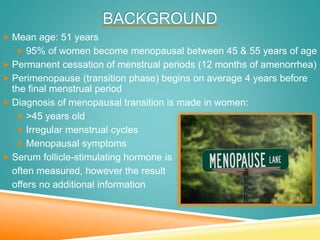
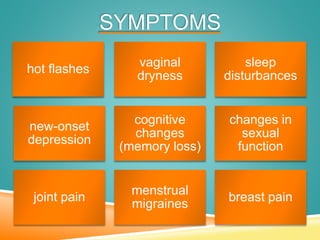
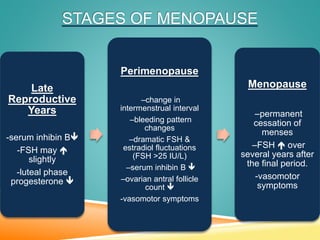
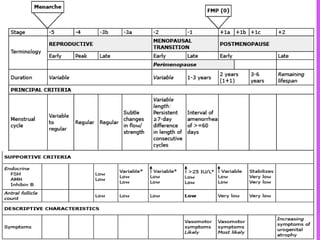
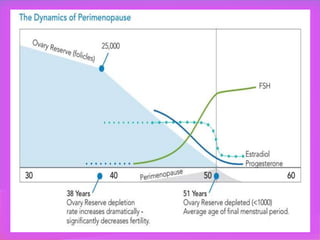
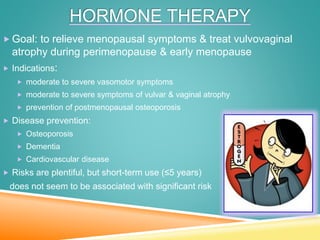
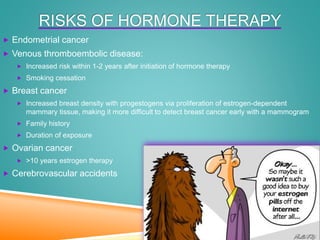
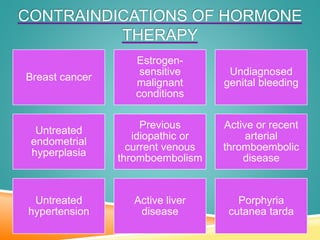
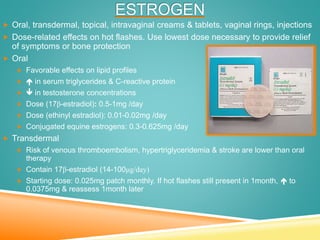
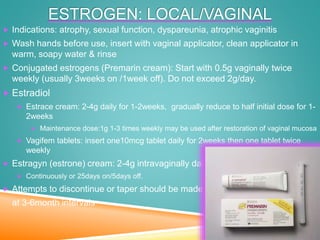
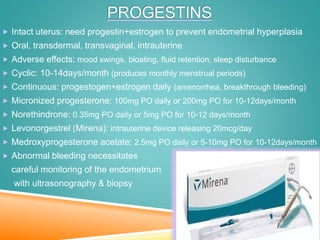
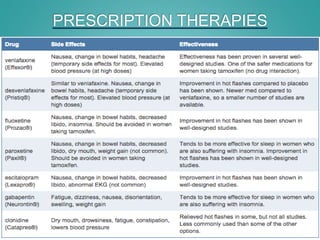
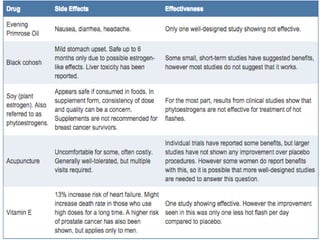
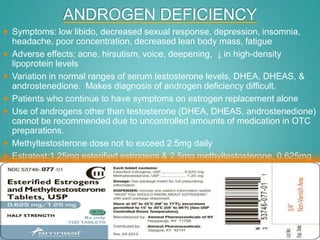
Menopause is the permanent cessation of menstrual periods, occurring on average at age 51. Hormone therapy can relieve menopausal symptoms but carries risks like endometrial cancer and blood clots. Options include oral or transdermal estrogen with or without progestin. Non-hormonal treatments include black cohosh, exercise, and lifestyle changes. Hormone therapy is generally recommended for short-term use to treat moderate to severe symptoms.