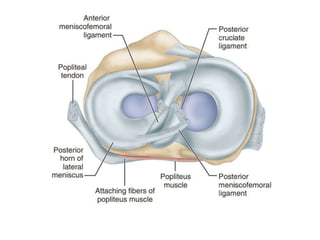
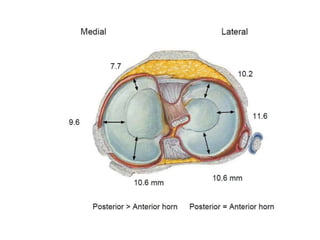
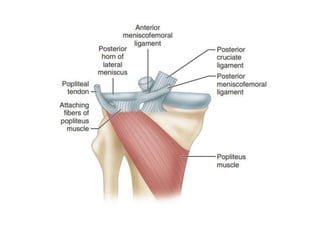
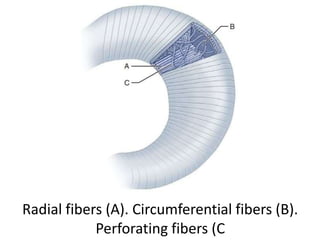
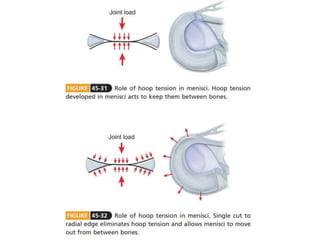
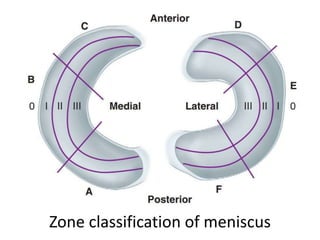
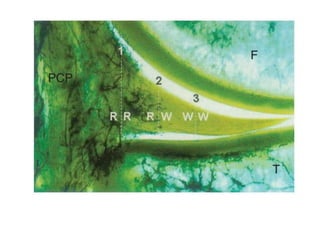
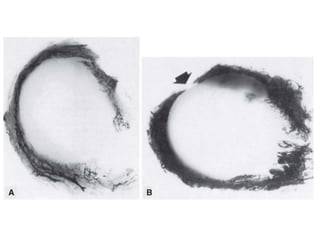
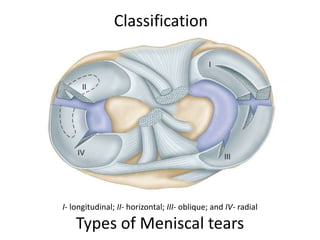
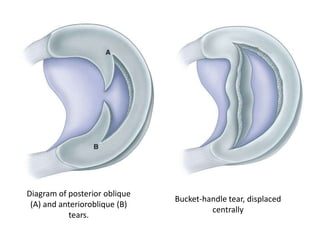
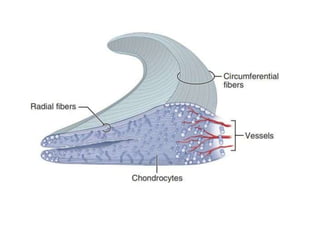
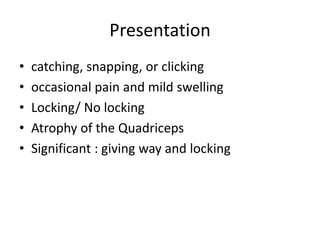
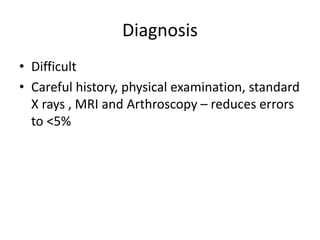
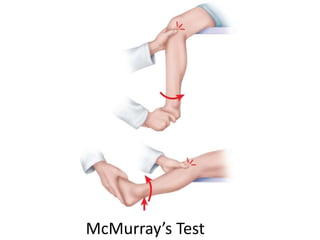
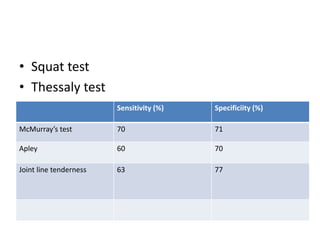
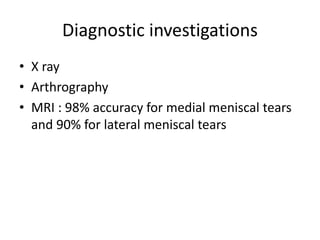
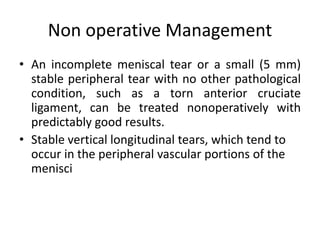
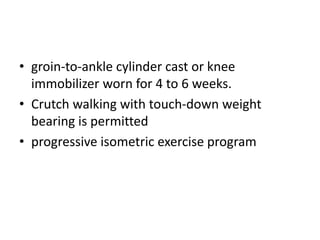
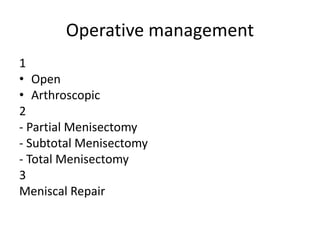
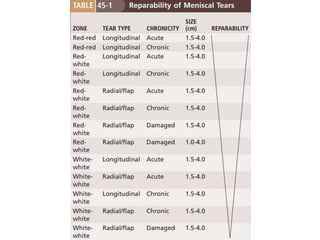
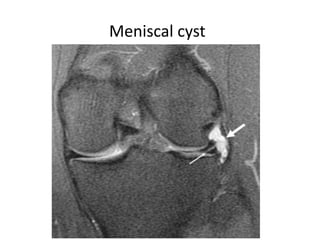
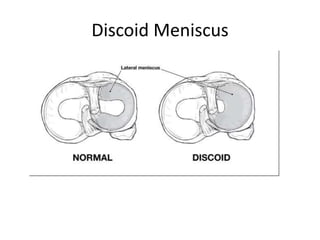
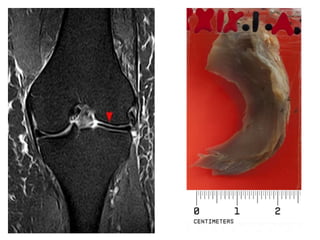
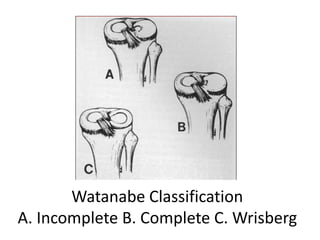
The meniscus has a crescent shape and acts as a shock absorber in the knee. It develops fully by 10 weeks of gestation. The meniscus has radial, circumferential, and perforating fibers that allow it to bear loads and stabilize the knee joint. Meniscal tears most commonly occur in the posterior horn from rotational forces on a flexed knee. Tears are classified as longitudinal, horizontal, oblique, radial, or displaced. Clinical exams like McMurray's test and MRI are used to diagnose tears, which are often treated surgically with repair, partial/subtotal/total meniscectomy. Untreated tears can lead to meniscal cysts or discoid meniscus formation over time