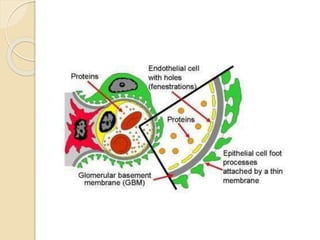
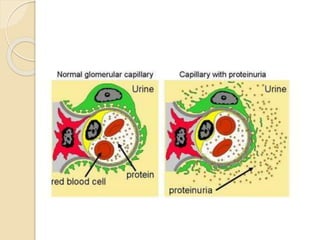
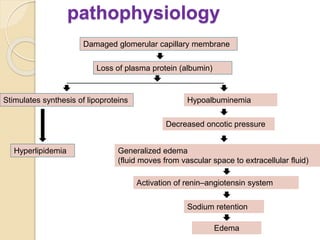
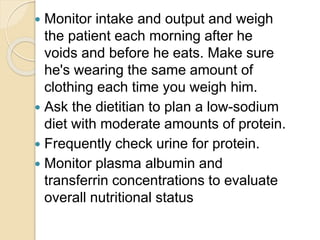
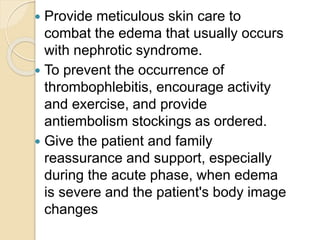
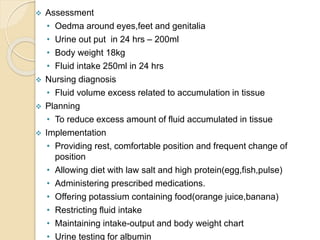
Nephrotic syndrome is a common cause of hospitalization in children, characterized by edema, hypoalbuminemia, and proteinuria. It can be congenital, idiopathic/primary, or secondary. The idiopathic type is most common and responds to immunosuppressants. Clinical features include edema, weight gain, reduced urine output, and increased risk for infection. Nursing focuses on managing fluid balance, preventing infection, improving nutrition, and providing education and support.