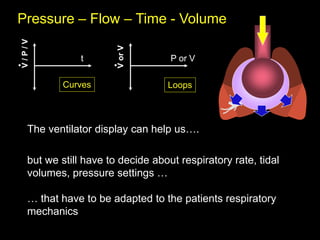
This document discusses basic respiratory mechanics relevant for mechanical ventilation. It covers topics such as volume change over time, gas flow, pressure differences, compliance, airway resistance, and the mechanical response to positive pressure application. Equations of motion relating pressure, volume, compliance, and resistance are presented. The effects of varying time constants on lung volume change over time are explored. Optimizing settings like tidal volume, inspiratory time, and expiratory time based on a patient's respiratory mechanics is discussed. The relationship between airway pressure, alveolar pressure, transpulmonary pressure, and chest wall elastance is also examined.









































![PPl = Paw x [E CW / (E L + E cw)]
Ptp = Paw x [E L / (E L + E cw)]
when airway resistance is nil (static condition)
Palv = PPl + Ptp Etot = EL + Ecw
Pairways (cmH2O)
Ppleural (cmH2O)
Ptranspulmonary (cmH2O)](https://image.slidesharecdn.com/1basicsonmechanicalventilation1-240328165001-78e0bd81/85/1-Basics-on-mechanical-ventilation-1-ppt-42-320.jpg)
![PPl = Paw x [E CW / (E L + E cw)]
Ptp = Paw x [E L / (E L + E cw)]
when airway resistance is nil (static condition)
Paw = PPl + Ptp
Etot = EL + Ecw
Gattinoni L
Critical Care 2004,
8:350-355
soft stiff](https://image.slidesharecdn.com/1basicsonmechanicalventilation1-240328165001-78e0bd81/85/1-Basics-on-mechanical-ventilation-1-ppt-43-320.jpg)
![In normal condition: EL = Ecw
Ecw/ Etot = 0.5 and EL/ Etot = 0.5
PTP ~ 50% of Paw applied
In primary ARDS: EL > Ecw (EL / Etot > 0.5)
Stiff lung, soft thorax PTP > 50 % of Paw applied
In secondary ARDS: EL < Ecw (EL / Etot < 0.5)
Soft lung, stiff thorax PTP < 50 % of Paw applied
In ARDS: PTP ~ 20 to 80% of Paw applied
Ptp = Paw x [E L / (E L + E cw)]](https://image.slidesharecdn.com/1basicsonmechanicalventilation1-240328165001-78e0bd81/85/1-Basics-on-mechanical-ventilation-1-ppt-44-320.jpg)