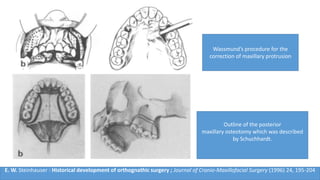
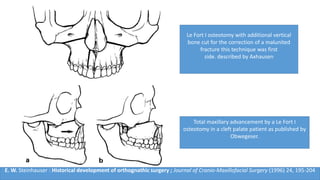
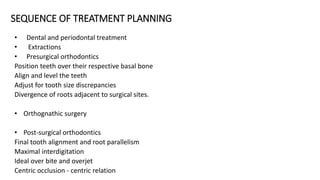
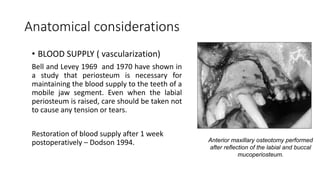
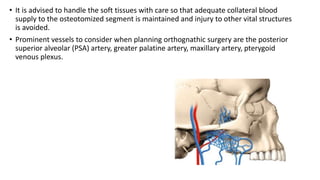
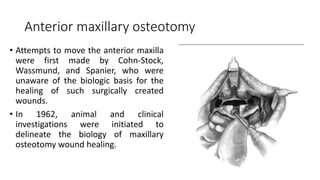
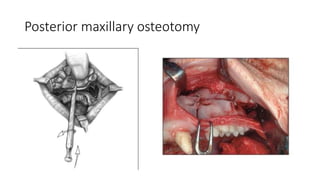
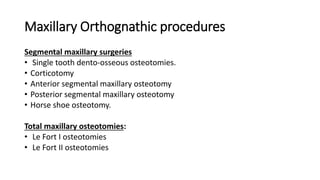
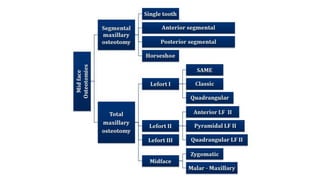
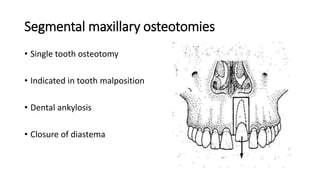
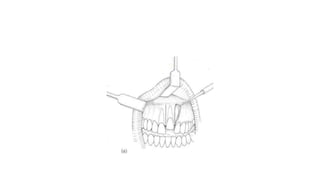
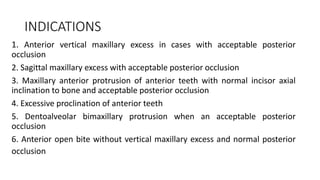
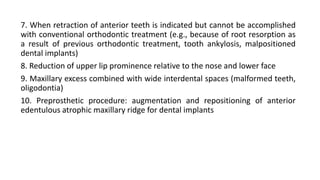
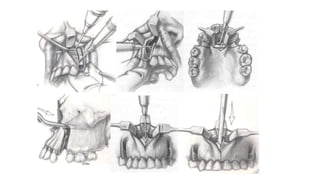
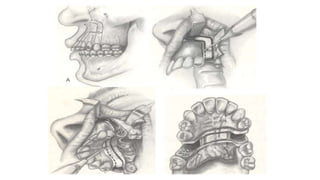
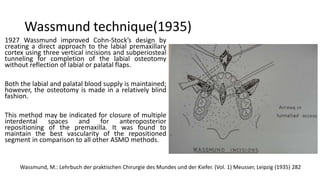
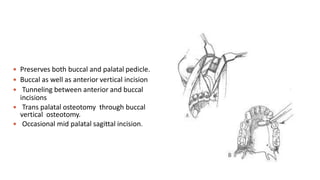
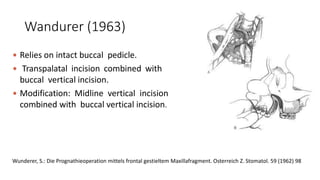
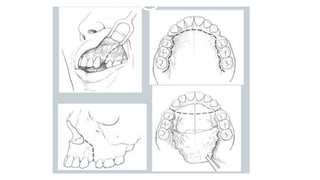
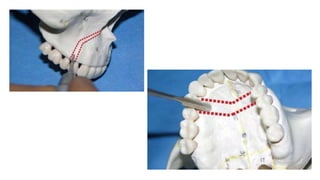
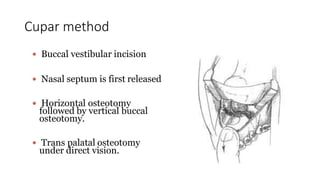
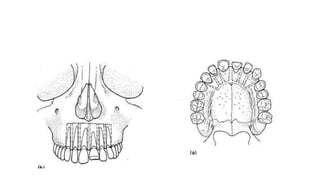
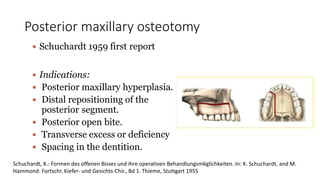
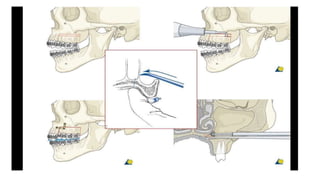
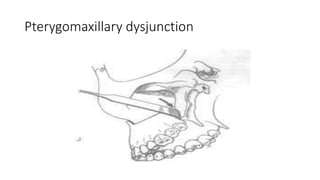
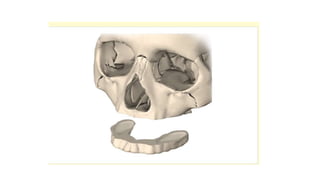
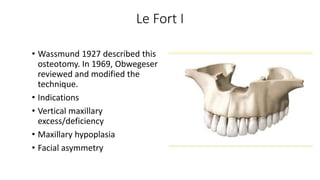
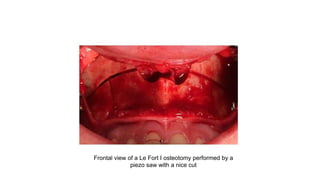
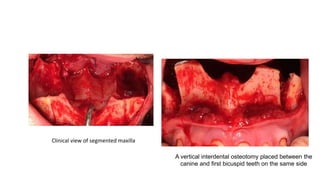
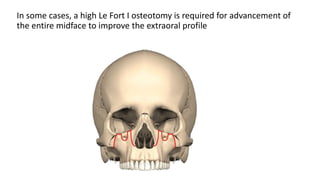
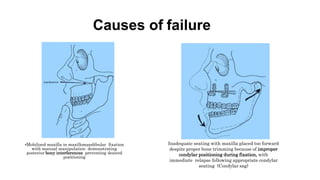
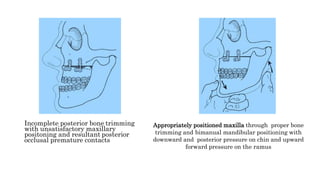
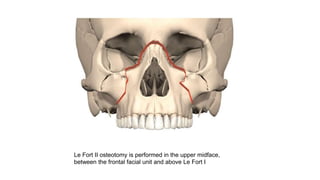
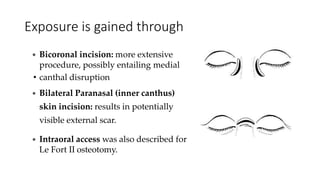
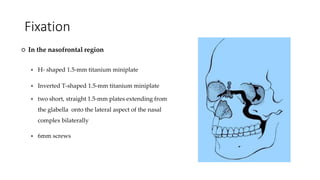
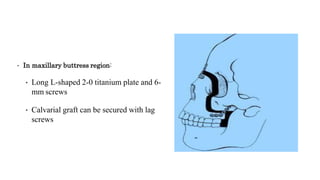
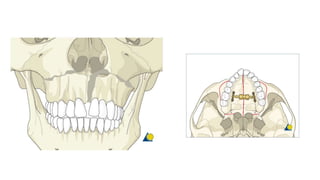
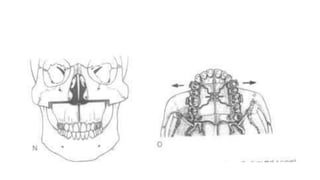
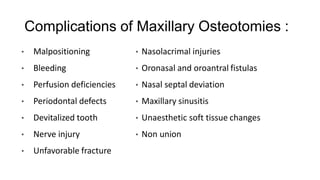
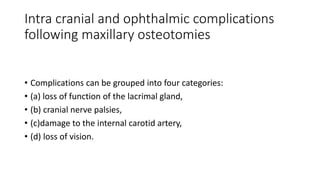
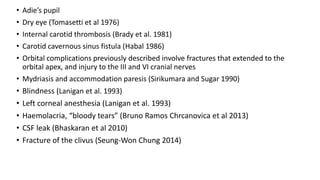
The document outlines maxillary orthognathic surgery, focusing on its definition, history, goals, and procedures such as Le Fort osteotomies. It discusses anatomical considerations, complications, and emphasizes the importance of wound healing in surgical outcomes. The text also encapsulates various surgical techniques, indications, and historical developments in orthognathic surgery, providing a comprehensive overview of the subject.