Maxillary osteotomy
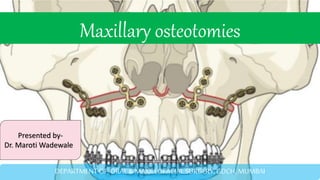
- 1. Maxillary osteotomies Presented by- Dr. Maroti Wadewale DEPARTMENT OF ORAL & MAXILLOFACIAL SURGERY, GDCH, MUMBAI
- 2. CONTENTS :- Introduction History Applied Anatomy Biological basis Le fort I Modifications Anterior sub-apical osteotomy Posterior sub-apical osteotomy Le fort ll Le fort lll Conclusion References
- 3. INTRODUCTION o Osteotomy- the surgical cutting or dividing of bone, usually to correct a deformity o Dentofacial deformities affect 20% of the population. o Maxilla can be mobilized and repositioned and the healing continues as long as the mobilizes maxilla is pedicled on broad soft tissue base (soft palate, lateral pharyngeal wall, buccal mucosa). o Le Fort I osteotomy is a commonly performed maxillary procedure for the correction of dentofacial deformity.
- 5. Hullihen SP. Case of elongation of the under jaw and distortion of the face and neck, caused by a burn, successfully treated. The American journal of dental science. 1849 Jan;9(2):157. HISTORY
- 6. Von Langenback B: Beitrage zur Osteoplastik- Die Osteoplastiche Resektion des Oberkiefers, Dtsch Klin Berl 48:471, 1859. Cheever DW: Naso-pharyngeal polyps attached to the basilar process of occipital and body of sphenoid bone successfully removed by section, displacement, and subse- quent replacement and reunion of the supe- rior maxillary bone, Boston Med Surg J 8:161, 1867. Wassamund M: Fracturen and luxiationen des Gesichsschadells, Berlin, 1927 Von Lagenbeck 1859 – procedure for nasopharyngeal polyps. He did not realize it, but he performed 1st orthognathic surgery Cheever 1867 performed a bilateral hemimaxillary down-fracture known as the “double operation,” which resembled a Le Fort I osteotomy, to remove nasopharyngeal pathology. Wassmund 1927 reported his initial attempt to perform maxillary osteotomy for correction of the open-bite deformity. Obwegeser 1965 started to perform maxillary surgery and described a large series of LeFort I osteotomies in 1969.
- 7. SURGICAL ANATOMY • Osseous structures • Vascular structures
- 8. infraorbital foramen is located between 8 and 20 mm from the nasal floor During osteotomy of the lateral nasal wall, care is taken to extend the osteotomy no farther than 25 to 30 mm posteriorly from the piriform rim. The mean length of the medial sinus wall from the piriform rim to the descending palatine canal is approximately 34 mm.
- 9. Nasolacrimal duct:- Located within the bony wall between maxillary sinus & nasal cavity Terminates below the inferior turbinate in the inferior meatus meatus of the nasolacrimal duct is unlikely to be injured if the osteotomy is made just beneath the infraorbital foramen and into the piriform rim at the level of the inferior turbinate. Location: 10-14mm behind piriform rim 10-21 mm above nasal floor Bell WH: Modern practice in orthognathic and reconstructive surgery , Philadelphia, 1992, WB Saunders.
- 11. VASCULAR ANATOMY Blood supply of the maxilla. (A) Nasopalatine artery, (B) Descending palatine artery, (C) Greater palatine artery, (D) Lesser palatine artery, (E) Maxillary artery, (F) Ascending pharyngeal artery, (G) Ascending palatine artery, (H) Facial artery, (I) External carotid artery, (J) Le Fort I downfracture. Teemul TA, Perfettini J, Morris DO, Russell JL. Post-operative avascular necrosis of the maxilla: a rare complication following orthognathic surgery. Journal of surgical case reports. 2017 Jan
- 12. The internal maxillary artery enters the pterygopalatine fossa approximately 16 mm above the nasal floor. A large descending palatine artery, which is the major vessel encountered most commonly during maxillary osteotomies, descends through the hard palate as greater and lesser palatine arteries. Distance of descending palatine artery from tuberosity: 10mm The average distance from the most inferior point of the pterygomaxillary junction to the posterior superior alveolar artery is 15 mm, to the infraorbital artery is 32 mm, and to the descending palatine artery is 25 mm. Bell WH: Modern practice in orthognathic and reconstructive surgery , Philadelphia, 1992, WB Saunders.
- 13. BIOLOGICAL BASIS FOR ORTHOGNATHIC SURGERY Within three weeks the circulation between all of the sectioned bone fragments had been reconstituted. The pulp canals of several teeth adjacent to the ver- tical interdental bone cuts were not vascu- larized because their apical blood supply was severed. The dental alveolar segments were freely mov- able one week after surgery and slightly movable after three weeks.
- 14. When the descending palatine artery are severed during maxillary osteotomy the blood supply of maxilla is preserved via Ascending Pharyngeal, Ascending Palatine & Soft Palate Vessels Preservation of the integrity of the incisive canal or greater palatine arteries was not essential to maintain circulation to the anterior or posterior maxillary dental alveolar segments Twenty-four weeks after maxillary osteotomies, the periosteal and endosteal circulatory beds had been virtually reconstituted to their normal vascular architecture.
- 17. INDICATIONS OF LE FORT I OSTEOTOMY Vertical maxillary excess Vertical maxillary deficiency A-P maxillary deficiency(maxillary hypoplasia) Post trauma patient
- 19. STEPS IN LE FORT 1 OSTEOTOMY o Preoperative preparation o Mucosal incision & subperiosteal dissection o Placement of reference marks o Anterior buccal osteotomy o Posterior buccal osteotomy o Separation of nasal septum from septal crest of maxilla o Pterygomaxillary separation o Down fracture of maxilla o Mobilization of maxilla o Reduction of the palatal aspect of nasal septum o Turbinectomy o Stabilization of the repositioned maxilla o Closure
- 20. PRE –OPERATIVE Patient position Head elevated at 10-15 degree/reverse trendelenberg position. Modified hypotensive anaesthesia MAP by increasing the amount of inhaled anesthetics such as sevoflurane, isoflurane, and desflurane. (systolic BP 100) Kademani D, Tiwana P. Atlas of oral and maxillofacial surgery. Elsevier Health Sciences; 2015 Apr 9.
- 21. EXTERNAL REFERENCE MARK Kirschner wire • Kirschner wire at nasal bridge • external reference markers have been shown to be more accurate • Screw In Nasion • The medial palpebral fissure also can be used as a reference point instead of a metallic marker. • Kahnberg et al found no statistically significant difference between the two methods. Bell WH: Modern practice in orthognathic and reconstructive surgery , Philadelphia, 1992, WB Saunders.
- 23. INFILTRATION OF LA AND INCISION • LA with vasoconstrictor is injected into upper labial/ buccal sulcus • 1:100000 • Palatal injection are unnecessary. • 5 mm above mucogingival junction, Electrocautery discouraged-
- 24. Anterior:- -Septopremaxillary ligament from ANS -The nasal mucosa is reflected from the floor posteriorly upto 15 – 20 mm from aperture and from the lateral nasal wall Superio-lateral- zygomatic body Posterior:- -Tunneled to preserve mucosal pedicle -Care is taken to maintain the integrity of periosteum and prevent herniation of BFP in surgical field
- 25. PLACEMENT OF INTERNAL REFERENCE MARKS • Osteotomy line is demarcated by drilling holes in lateral maxillary walls 5-6 mm above the apices of maxillary canine and 1st molar
- 26. ANTERIOR BUCCAL OSTEOTOMY •Zygomaticomaxillary buttress along the lateral wall of maxilla and till piriform aperture. •It terminates below inferior turbinate. To avoid damage to nasolacrimal duct •Parallel to occlusal plane •With saw / rotary burs / piezo
- 27. IN DEPTH • Should not be extend beyond 25-30mm from the piriform rim posteriorly to avoid the injury to Descending Palatine Artery • Finally saw is reversed to make a cut in sinus from inside out in posterior wall of maxilla • In superior repositioning The Maxilla:- Drill holes are made superior to the first osteotomy line at a distance measured by small caliper. Finally saw is used to connect these points.
- 28. POSTERIOR BUCCAL OSTEOTOMY • From the ZM buttress to the tuberosity .It is sectioned under the mucosal tunnel with direct visualization • 3mm lower than anterior osteotomy .Directed inferiorly to prevent the injury to maxillary artery or its branches. • 5mm superior to the 2nd molar
- 29. 3RD MOLAR IN POSTERIOR OSTEOTOMY…. Presence of 3rd molars should not alter the osteotomy designs. Extraction indicated :- Exposed during osteotomy Interfere with repositioning
- 30. REPEAT THE PROCEDURE ON OPPOSITE SIDE
- 31. Osteotomy of lateral nasal wall Guarded Osteotome is placed at piriform rim and directed posteriorly and inferiorly along the lateral nasal wall towards the perpendicular plate of palatine bone. Until audible change in malleting/ resistance is indicative of perpendicuar plate of palatine bone
- 32. NASAL SEPTUM OSTEOTOMY • Nasal septal osteotome is directed posteriorly & inferiorly, starting above the anterior nasal spine upto 25-30mm. • It frees the cartilagenous & bony septum and vomer from the superior surface of maxilla.
- 33. Complete sectioning of palatine bone should be accomplished, even if it results in damaging the descending palatine artery . Incomplete section can result in inadvertent fractures which may extend into orbit
- 34. • Techniques for pterygomaxillary seperation: • Obwegeser osteotome • Swan neck & shark fin modification of osteotomes • pterygoid chisel • Tessier spreaders ( by Precious et al) • J mobilizers PTERYGOMAXILLARY DYSJUNCTION Obwegeser osteotome Tessier spreader
- 35. Curved osteotome directed medially and anteriorly at the lowest part of pterygomaxillary junction. Excessive anterior angulation may increase the risk of injuring the descending palatine artery. Do not direct the tip of osteotome cranially Maxillary artery lies approx. 25mm above the base of the pterygomaxillary fissure Ostetome should be ranged in width 10-15mm Transmission of forces by the sphenoid bone to the base of skull may lead to loss of vision.
- 37. DOWN FRACTURE OF MAXILLA • Digital pressure is applied over the anterior maxilla. • If resistance is encountered, revise osteotomy cuts. • Do not use excessive force during downfracture • Probable reasons for failure of down-fracture: 1. The pterygoid plates & tuberosity are not sufficiently separated. 2. Lateral nasal wall osteotomy is incomplete.
- 38. OBILIZATION OF MAXILLA • Place the maxillary mobilizer bilaterally behind tuberosity & pull the maxilla forward & downward using cricoid hook/ J stripper place in the incisive canal. • DPA is visualised and bone must be removed carefully preserved/ ligated
- 39. Septoplasty and theReduction of theInferior Turbinates
- 40. BonyInterferences • All bony interferences and premature contacts must be adjusted. • Most likely the area of interference is the maxillary tuberosity and posterior maxillary wall.
- 41. section of the maxilla to demonstrate the bony cuts.
- 42. MAXILLOMANDIBULAR WIRE FIXATION • The mobilized maxilla is seated in prefabricated occlusal splint and IMF is applied. • Check the reference marks for accurate maxillary positioning
- 43. • Planned vertical relationship is established. • Position of condyle in glenoid fossa should be checked. Digital pressure anterior to mandibular angle in upward and anterior direction • Make sure there are no bony interference during the rotation Positioning of the condyle in glenoid fossa
- 44. INTRAOPERATIVE DIAGNOSIS OF CONDYLAR SAG
- 45. STABILIZATION OF THE REPOSITIONED MAXILLA Non – rigid Trans-osseous wiring IMF – 4-6 months Rigid/semi rigid Metal Plates Resorbable plates Position screws Mesh IMF- 4-6 weeks
- 46. RIGID V/S NON-RIGID FIXATION • Rigid Iinternal Fixation improves stability of maxillary osteotomy. • Surgeon employing rigid fixation technique must be exacting as this techinque is less forgiving for postoperative adjustments. • Plate and screw lacks flexibility and skeletal adjustments and all the occulsal changes required postoperatively are accomplished solely through dental movements. • Surgeon must ensure that the plates are precisely adapted to contour the maxillay bony walls because forcing non-contoured plates against the bone may result in displacement of bony segments as the screws are tightened.
- 47. • Skeletal suspension described by Epker and Fish -- great postoperative flexibility with regard to skeletal adjustments. • Multidimensional movements can be accomplished by selective tightening or loosening of skeletal suspension wire Maxillary advancements upto 5mm have shown to be stable regardless of type of fixation used to stablise the maxilla.
- 51. BONE GRAFTING Le Fort 1 osteotomies using rigid fixation and interpositional PBHA grafting during bimaxillary surgery is a stable procedure with good predictability in cleft and non-cleft patients, regardless of the direction of vertical maxillary movement.
- 52. Graft Functions -Osteotomy stablisation -Horizontal augmentation of infraorbital region and zygoma. Transosseous orbital rim-pirifrom rim suspension wire o Iliac crest graft o Graft notched superiorly to accommodate ION o Corticocancellous block fits as an onlay interpositional block on the infraorbital rim and body of zygoma o Transossoue wire is tightened. Ti miniplates and screws are placed between the graft and advanced maxilla Body of zygoma Piriform rim
- 53. CLOSURE • Alar base cinch • A slowly resorbing suture (e.g., 2- 0 polyglycolic acid) Nasalis muscle are grasped and suture is passed through each muscle in the superior aspect of flap & sutured to the muscles in the inferior limb of incision.
- 54. If the tissue bulk in the inferior part of flap is inadequate to support the suture, a hole can be drilled through the ANS & a cinch suture can be placed
- 56. V-Y CLOSURE • Helps in maintaining the height of exposed vermilion & lip length • A skin hook is placed in the midline to create an “inverted T” closure of approximately 1 cm length. • When mucosa is closed suture should grasp the thinnest layer of tissue
- 57. MODIFICATION IN LE FORT-I OSTEOTOMY
- 59. MAXILLARY QUADRANGULAR LE FORT I OSTEOTOMY Historical review 1st described by Obwegeser as a LeFort-I osteotomy in which osteotomy was placed “as high as possible,from the tuberosity area arround the whole maxilla, staying just beneath the infraorbital foramen.”
- 60. SURGICAL INDICATIONS Pts with maxillary-zygomatic deficiency ,class III skeletal malocclusion with normal nasal projection. Pts with normal nasal projection with infraorbital and zygoma deficiency (desiring reduced surgical morbidity).
- 61. • Osteotomy :- Horizontal osteotomy begins from piriform rim at level of infraorbital nerve extending laterally just inferior to the IOF to zygoma body. At this point it makes a right angle and proceeds inferiorly through the maxillary buttress and through the lateral antral wall to PtM fissure. Posteriorly osteotomy is completed at vertical wing of palatine bone just anterior to pterygoid plate with osteotome.
- 64. 1 weeks – increased periosteal-endosteal vascular supply , granulation tissue composed fibroblasts and capillaries. 2 weeks – osteophytic bone from periosteum and bony edges, blood vessels arising from endosteum, reattachment of soft tissue of underlying bone. 4 weeks – bony callus – maintains vitality of maxilla, active osteoblastic activity 6 weeks – soft tissue flaps completely reattached to underlying bone , callus shows mature bone. 12 weeks – osseous bridging between fragments appeared complete REVASCULARISATION AND HEALING IN ORTHOGNATHIC SURGERY
- 65. Complication OF Le Fort-I osteotomy
- 67. Source of bleeding: I. Lateral & medial pterygoid muscles II. Posterior superior alveolar artery III. Greater palatine artery IV. Terminal branches of maxillary artery V. Pterygoid venous plexus VI. Internal carotid artery HEMORRHAGE
- 69. Protocol for the Management of Postoperative Hemorrhage Rapid release of maxillo- mandibular fixation allows for clearing of intraoral and pharyngeal clots. If brisk ac- tive hemorrhage is occurring when the patient is first seen, large Foley catheters should be placed bilaterally to serve as temporary posterior nasal packs A tracheost omy should be considere d patient's general status should be quickly as- sessed, vital signs monitored, and intravenous fluids started approxim ate assessme nt of blood loss Coagulatio n studies should be done nasal area should then be examined with a good light source, Embolization of the internal maxillary artery and its distal branches should be considered if recurrent hemorrhage occurs Ligation of the external carotid or internal maxillary arteries is another possibility for the management of recur- rent arterial bleeding if therapeutic embolization cannot be performed
- 70. CONSIDERATION TO PREVENT BLEEDING IN LF-I OSTEOTOMY • Knowledge of the anatomy, especially that of the posterior maxilla & pterygopalatine fossa. • Careful and gentle surgical technique. • Proper completion of osteotomies before attempt an downfracturing of maxilla. • Avoiding application of excessive forces.
- 71. UNFAVOURABLE OSTEOTOMY • LeFort-I osteotomy requires separation of maxillary tuberosity from Pterygoid plate and pyramidal process of palatine bone as well as nasal septum. • Osteotomy at pterygo-palatine area is largely blind because the area can not be visualised before downfracture. Most Common type of unfavorably osteotomies • Fracture at the junction of horizontal process of palatine bone with the palatal process of maxilla. • High horizontal fracture of the pyramidal process of palatine bone • Horizontal fracture of pterygoid plates,both with or without separation from the tuberosity.
- 72. Trigemino-Cardiac Reflex • Sudden decrease in pulse rate (PR) and mean arterial blood (MABP) pressure that may consequently develop asystole and even cardiac arrest . • 1.6% during maxillofacial, temporomandibular,orthognathic surgeries. C/F :- Bradycardia less than 60 beats /min Hypotension. Theories:- 1. Anxiety 2. Anesthetic Agent(hypocapnia, hypoxemia) 3. Stimulation of lingual and palatal branches of TG nerve as the triggering factor. Sensory branches of TGN send signals from gasserian ganglion to sensory nucleus TGN. Which are then transferred to vagus motor nucleus through short nerves and directed to myocardium through cardiac branches of vagus nerve .
- 73. TRIGEMINO-CARDIAC REFLEX IN LE FORT-I OSTEOTOMY Management : Manipulation of maxilla should be stopped immediately Administration of anticholinergic drugs
- 74. Avascular necrosis The spectrum of vascular compromise ranges from loss of bony segment ,loss of teeth to loss of attach gingiva. Early sign: Blanching Cyanosis of attach gingiva and mucosa Etiology o Vascular insult to maxilla o Excessive manipulation of segments. o Hypoperfusion from prolong hypotensive anesthesia o The preservation of the integrity of the descending palatine arteries was not found to be essential to maintain circulation to the down-fractured maxilla. Management: • Returning the maxilla back to its original or intermediate position & checking for improved tissue colour & blood flow • Oral hygiene maintenance and systemic antibiotics to prevent secondary infection • Surgical debridement of necrotic tissue with the use of hyperbaric oxygen.
- 76. FACTORS RESPONSIBLE FOR SUCH COMPLICATIONS • Improper design of soft tissue incision • Excessive stretching of palatal soft tissue pedicle • Segementalization of maxilla • Extensive hypotension • Severance of descending palatine vessels
- 77. NON-UNION/DELAYED UNION Causes: • scarring due to previous surgery • Poor surgical planning • Para-functional habits • Posterior and superiorly positioned maxilla with poor bone contact • Systemic-diabetes, smoking • Prevention- • when unstable maxilla anticipated-boneplates+auxillary fixation • IMF:1-6weeks, skeletal wires • Use of bone grafts for large defects
- 78. treated with additional forms of fixation and/or immobilization. Currently, we use bone plates combined with suspension wires and 6 weeks of immobilization in many of these cases. Grafting has been advocated in the pterygomaxillary area; however, graft material also should be placed in large defects in the anterior and lateral maxillary wall areas.
- 79. RELAPSE Postoperative movement either towards the preoperative position or farther away from it. Proffit et al coined the phrase “Hierarchy of stability” in which they quantified relapse according to different types of procedure
- 81. UN STABLE MAXILLARY MOVEMENTS Transverse movement Inferior movement
- 82. • Maxillary superior repositioning -Mean relapse rate 11% to 3% from anterior and posterior maxilla,respectively,at mean follow up of 14 months. • Maxillary advancement:- -Relapse of 5-19% at average follow up of 15 months with RIF -It is proportional to amount of advancement. Bone grafting in advancement>8mm reduces relapse. • Maxillary inferior repositioning -28% and 70% relapse rate at anterior and posterior maxilla,at follow up of 14 months. • Maxillary transverse widening • Least stable – prolonged retention
- 83. NERVE INJURYInfra Orbital Nerve injury:- Injured due to traction and compression 6% Neurosensory deficient at 12 months when tested objectively all patients reported satisfaction with the surgical results, and would recommend the procedure to others. Descending/Greater Palatine Nerve injury -Nasopalatine, -Posterior, Middle, Anterior superior alveolar nerve are completely severed. -Despite ligation and division of neurovascular bundle, sensory recovery does occur and represent collateral axonal sprouting from adjacent nerve.
- 84. Post operative vision loss • Rare complication(0.25%)* Etiology 1. Postoperative intraorbital bleeding 2. Intraoperative Hypotension & hypoperfusion of the optic nerve: retina & optic nerve are sensitive to hypoperfusion or ischemia, it can only tolerate ischemia for 60-90 min.
- 85. MISCELLANEOUS abducens palsy, three cases of oculomotor palsy
- 89. incidence of 4.76% of maxillary sinusitis
- 91. ANTERIOR MAXILLARY SUB-APICAL OSTEOTOMY first anterior segmental maxillary osteotomy (ASMO) was reported at the beginning of the twentieth century. Günther Cohn-Stock
- 92. Indications • Bimaxillary protrusion with mandibular subapical osteotomy • Maxillary Prorusion • Ant open bite provided VME is not present • Orthodontic treatment is not feasible • Esthetic consideration Biologic basis BS anterior maxilla maintained by labial-buccal and palatal tissues Types (1) WASSMUND METHOD (2) WUNDERER METHOD (OUT #) (3) CUPAR METHOD (Down #)
- 93. WASSMUND METHOD Preserves both buccal and palatal soft tissue pedicles. Procedure 1) Vertical mucosal incision b/w 3 & 4 (gingival margin to level of anterior nasal floor.) (superior to the root apex of maxillary canine.) 2) Mucoperiosteum reflected to apical 3rd of max canine 3) Tunnel subperiostelly expose nasal piriform aperture 4) Extraction or presurgical space of 3 – 5 mm.
- 94. 5) Palatal mucosa reflected to just past the midline 6)Osteotomy – bony cuts done leaving 2mm over the adjacent teeth 7)Bone in midpalatine region is thick, sometimes a midpalatal incision may be required.
- 95. • Repeated on opposite side • Dentoalveolar segment disarticulated from nasal septum • Anterior midline mucoperiosteal incision reflected ….nasal septal osteotome malleted above nasal spine to free the segment from the septum. • After mobilising placed into occlusal splint. • Palatal soft tissue pedicle checked for any folds, compromising the blood supply
- 96. WUNDERER METHOD Facial soft tissue incisions similar to wassmund’s method# Mucoperiosteal incision transversely across palate (anterior to the planned osteotomy site) Palatal mucosa posterior to the incision elevated Pre planned extraction performed …. Osteotomy upto the anterior nasal aperture done Note : Facial portion osteotomy is done first and adequacy of perfusion of facial soft tissue pedicle confirmed first , then proceed with palatal osteotomy else as a second stage procedure
- 97. • If superior repositioning required, access to junction of ANS and nasal septum poor. • A vertical incision can be made over the anterior nasal spine, (but Labial flap represents total blood supply to the anterior maxilla, it is not recommended. Advantages • Direct palatal access - ability to create transverse osteotomy through a molar site • Relies on intact buccal pedicle for blood supply. • Separation of nasal septum performed easily. • Modified to include midline vertical incision to achieve access to horizontal osteotomy through a sub-periosteal tunnel connected with the vertical incisions at extraction site
- 98. CUPAR METHOD • Commonly used technique • Minor version of total maxillary osteotomy • Buccal vestibular incision is created allowing direct access – anterior lateral maxilla piriform aperture nasal floor and sepum
- 99. ADVANTAGES OF CUPAR’S TECHNIQUE 1. Direct access to nasal structures 2. Unhampered access to superior maxilla – reduction of vertical maxillary excess / Bone grafting in downward cases. 3. Ability to remove palatal bone under direct visualization. 4. Preservation of blood supply palatal pedicle 5. Ease of placement of RIF.
- 101. Schuchardt , 1959 Indications • Posterior maxillary alveolar hyperplasia • Total maxillary hyperplasia • Distal repositioning of posterior segment • Anterior repositioning of posterior segment • Transverse excess or deficiency • Posterior open bite
- 102. INCISION DESIGN 1) Horizontal vestibular incision from canine to 2M below zygomatic buttress with tunneling access 2) Mucoperiosteum reflected superiorly leaving inferior intact 3) Horizontal osteotomy followed with vertical osteotom
- 103. TRANSANTRAL OSTEOTOMY High palatal vault permits palatal osteotomy transantrally beneath the nasal floor. A, Transantral osteotomy is made at the junction of the horizontal palate and vertical alveolar process. B, Approach for deep vaulted palates. - the transantral cut is completed along the entire anteroposterior extent of the planned palatal osteotomy except in the area of the descending palatal neurovascular bundle. C, Approach for flat shallow palates. Patients with low flat palatal vaults are more easily osteotomized through the nasal floor
- 104. Pterygomaxillary disjunction with a curved osteotome Down fracturing using digital pressure.
- 105. • orthodontic stabilizing arch wire can be inserted into buccaI headgear tubes to further stabilize the posterior dento-alveolar segment • Rigid fixation is applied • When the patient has multiple missing teeth or when lateral expansion of more than 5 to 7 mm of the maxillary segment has occurred transpalatal orthodontic stabilization should be considered • Closure of soft tissue incisions is done • When lateral expansion does not leave enough palatal tissue for closure, additional mucoperiosteal incisions on the contralateral palate may be required to mobilize palatal tissue so that mucosa can be closed over the palatal osteotomy site.
- 106. SURGICALLY ASSISTED MAXILLARY EXPANSION • Assists to correct deformities in transverse dimension. • First described by Angell in 1860 • This procedure is in essence combination of distraction osteogenisis and controlled soft tissue expansion. Diagnosis and clinical evaluation: • Para nasal hallowing • Narrowed alar base • Deepening of nasolabial folds • Zygomatic deficiency ngell, E. H.: Treatment of irregularities of the permanent or adult teeth, Dent. Cosmos 1: 540-544, 1860.
- 107. Treatment options based on skeletal maturity • Slow dentoalveolar expansion • Orthopedic rapid maxillary expansion • SAME • Segmental maxillary osteotomy Advantages of SAME • improved stability • non extraction alignment of dentition • elimination of negative space • improved periodontal health and nasal respiration
- 108. Indications: • skeletal discrepancy greater than 5mm associated with wide mandible • failed orthodontic expansion • extremely thin, delicate gingival tissue • significant nasal stenosis. • More than 7 mm of expansion Technique: • First the mandibular dentition should be decompensated • Expansion appliance should be placed preoperatively
- 109. Step 2: Buccal Osteotomy Step 2: Buccal Osteotomy Step 1: Incision Step 4: Palatal Osteotomy Step 4: Palatal Osteotomy Step 5: Midline Osteotomy
- 110. • Maxilla should remain stationary for 5 days postoperatively. • Pt should feel discomfort while activation. • Expansion at a rate of 0.5 mm/day • Over correction is not recommended. • Retention: 6 to 12 months after expansion
- 111. SINGLE TOOTH OSTEOTOMY Indications Tooth malposition Dental ankylosis Closure of a diastema Biologic basis Collateral circulation within maxilla surrounding soft tissue envelope are adequate. Freely anastomosing vessels gingiva palate floor of nose periodontal plexus network allows maintenance of blood supply One or more teeth and their supporting bone can be moved as a segment.
- 112. LE FORT II OSTEOTOMY
- 113. HISTORY • 1970, Converse and associates described a pyramidal nasoorbital maxillary osteotomy that approached le fort ll osteotomy in concept • 1973, Psillakis and associates gave the modified pyramidal naso-orbital maxillary osteotomy • 1973, Henderson and Jackson , described the le fort ll osteotomy closely following the fracture pattern.
- 114. Surgical access to nasoorbital component: Two oblique incisions on either side of the nose over the frontal process of maxilla/ dorsal nasal incision Alternatively , bicoronal flap combined with infraorbital or conjuctival approach SURGICAL TECHNIQUE
- 115. • Sub-periosteal dissection carried out to expose nasal bridge and medial orbital walls until the anterior and posterior lacrimal crest • Medial canthal ligament should not be disturbed • Periosteum from medial orbital floor raised to meet the medial wall dissection behind the lacrimal sac • Sac and duct raised from their bony attachments
- 116. • Transverse cut made through nasal bone below the known position of cribriform plate(crista galli) • Cut extended into medial wall of orbit just below the medial canthal attachment across upper part of lacrimal groove and just through posterior lacrimal crest • Second cut made along orbital floor between lacrimal duct medially and infra-orbital canal laterally • The two cuts connected by a small chisel behind the lacrimal groove
- 117. • The osteotomy is continued down the anterior aspect of maxilla well past the infra- orbital nerve • From this point, posterior and lateral parts of the osteotomy are completed as for le fort l through intra-oral incision • Separating the maxilla from the pterygoid plates as in le fort 1 procedure
- 118. • Maxilla is disimpacted using Rowe’s disimpaction forceps for initial separation and mobilized freely using a Tessier’s maxillary mobilizers • It is then advanced according to pre- operative plan • Fixed using miniplate osteosynthesis
- 120. Henderson, D., I. T. Jackson: Nasomaxillaryhypoplasia- theLeFortIIosteotomy.Brit.J.oralSur g.11(1973)77◊◊
- 122. HISTORY • 1950, Gillies published an account of the first high maxillary osteotomy to correct middle face deficiency secondary to craniostenosis • 1957, Longacre used onlaid autogenous rib grafts for improvement of total mid-face deficiency • 1967, Paul Tessier reported that mobilization and expansion of the entire midface by means of a sub-cranial le fort lll osteotomy was possible
- 123. INDICATIONS • Underdevelopment of entire mid-face • Flat/sunken appearance of mid-face • Short nasal structure • Deficient nasal bridge • Exaggerated flatness of nasofrontal region • Reduced size of orbit • Exophthalmos • Retro position of zygoma • Syndromic patients: Crouzon, Apert etc
- 124. • Exposure of the middle face: • Bilateral maxillary vestibular incisions, bilateral inferior eye-lid incisions and either a bicoronal flap or incisions over dorsum of the nose • Periorbita is dissected approx 10mm deep into both orbits, lacrimal apparatus identified and protected.(no tearing of orbital fat) SURGICAL TECHNIQUE Kademani D, Tiwana P. Atlas of oral and maxillofacial surgery. Elsevier Health Sciences; 2SEBASTIANI AM, REBELATTO NL, KLÜPPEL LE, COSTA DJ, ANTONINI F, MORAES RS. Le Fort III osteotomy for
- 125. • Nasofrontal osteotomy carried out below the level of cribriform plate and above the horizontal orbital axis to minimize intra-cranial involvement • Osteotomy proceeds in the medial orbital wall above the lacrimal apparatus and attachment of medial canthal tendon extending 1cm into the orbit
- 126. • Osteotomy of lateral orbital rim begins with direct visualisation of orbital and temporal sides of lateral orbital rim and wall • Osteotomy proceeds posteriorly and inferiorly from anterior extent of FZ suture to zygomatic buttress. • Within the orbit, osteotomy is carried inferiorly and posteriorly into inferior orbital fissure. • Osteotomy carried across the orbital floor joining the osteotomy of the medial wall and that of lateral wall in the inferior orbital fissure carefully preserving the infra-orbital nerve
- 127. • Next, pterygoid plates freed from the maxilla via intra-oral vestibular approach • Final osteotomy is separation of perpendicular plate of ethmoid and vomer from the cranial base • Osteotome angled posteriorly and inferiorly along the slope of cranial base to avoid fracture of cribriform plate and intra-cranial involvement • Patency of all cuts tested and rowe’s disimpaction forceps used to mobilize the mid-face
- 128. • Mid-face skeleton must rest passively in the forward position in the pre- formed occlusal splint • Accurately pre-pared grafts are placed along zygomatic buttress defects, lateral orbital rim and wall defects, nasofrontal defects, pterygomaxillary regions. • Fixation is carried out and operated site thoroughly irrigated and closed
- 129. CONCLUSION • The experiments of Rene Le Fort in 1901 contributed largely not only to the understanding of maxillofacial fractures but also laid the foundation of osteotomy lines used today for maxillofacial deformities. • The works of William Bell largely established the biologic basis of maxillary osteotomy and subsequently today with le fort ll and lll osteotomies a vast spectrum of craniofacial deformities can be corrected • The basic principles of surgery and our understanding of vascular anatomy continue to be the cornerstone while performing these osteotomies • Any violations of these basic principles will frequently lead to undesirable complications • Proper diagnosis and careful treatment planning will always provide efficient results to our patients
- 130. REFERENCES • Oral and maxillofacial surgery: .Fonseca: vol-2 • Peterson: vol-2 • Essentials of orthognathic surgery: Reyneke. • Maxillofacial surgery:Ward Booth: vol-2 • Atlas of Oral and Maxillofacial Surgery. • Contemporary Treatment of DENTOFACIAL DEFORMITY. • Orthognathic Surgery - Principles and Practice - Jeffrey C. Posnick