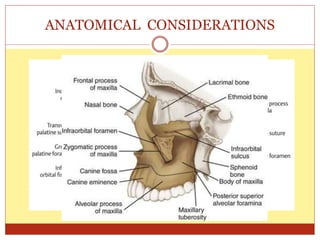
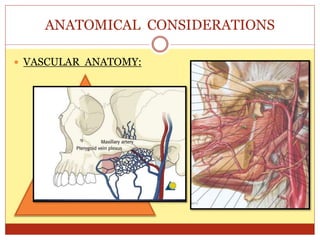
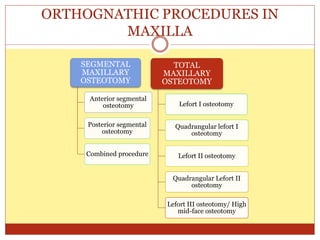
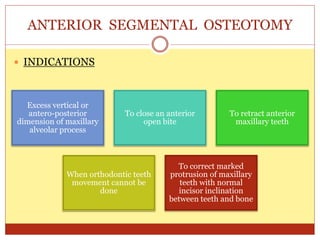
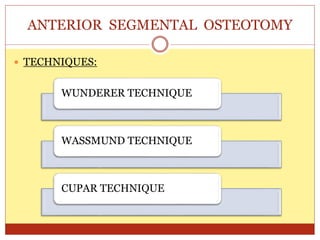
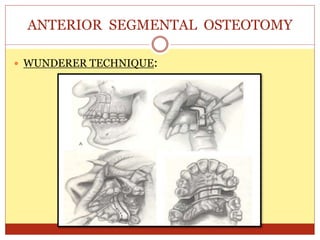
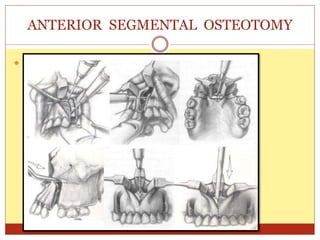
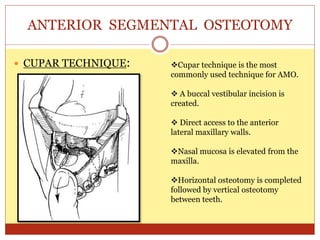
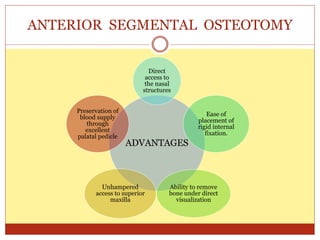
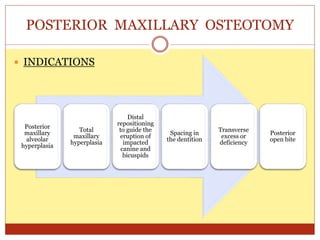
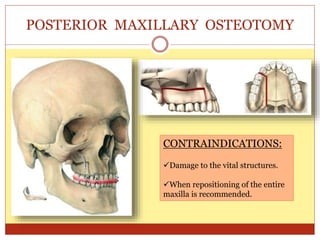
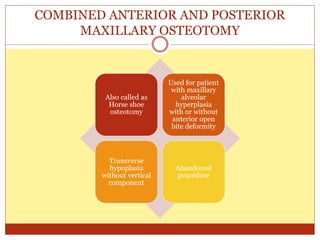
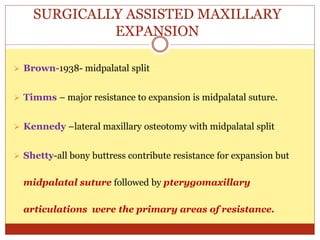
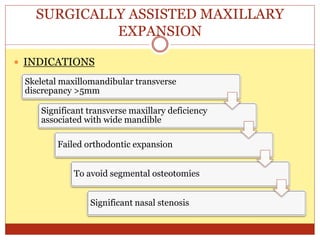
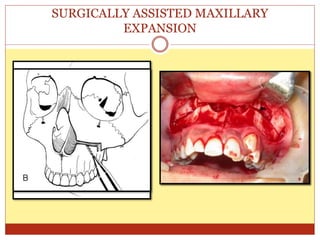
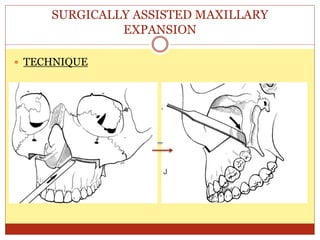
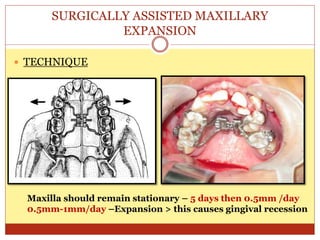
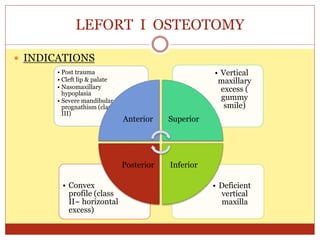
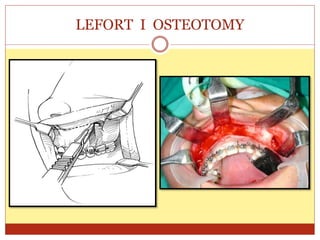
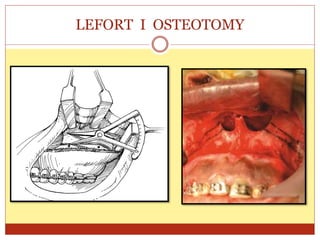
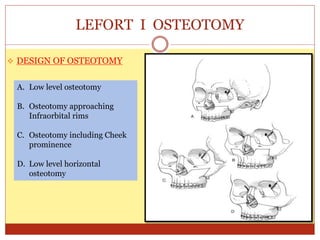
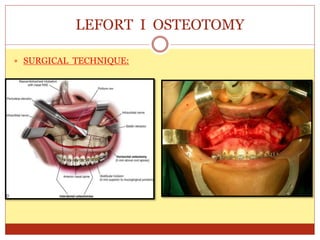
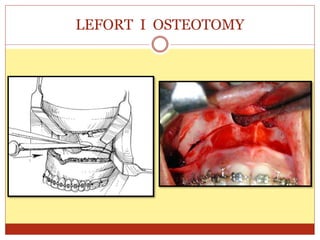
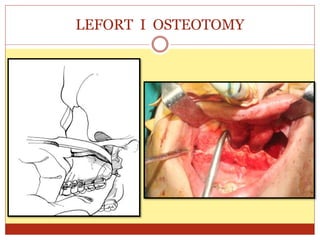
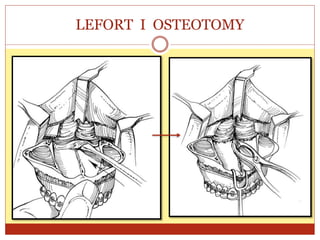
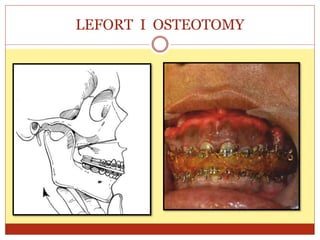
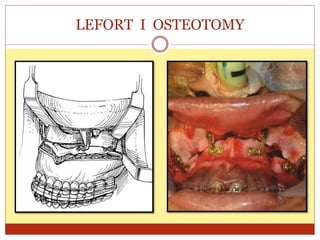
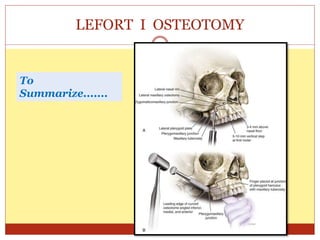
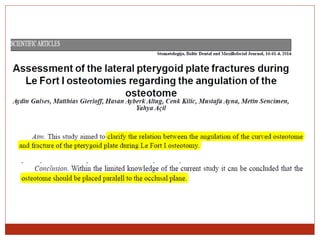
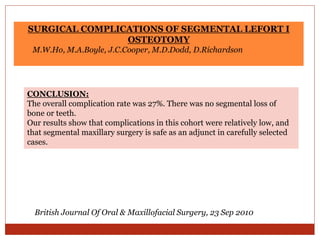
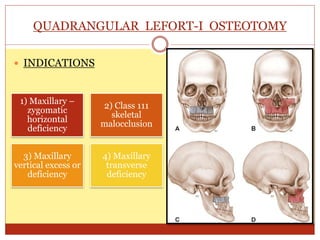
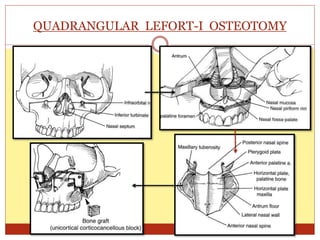
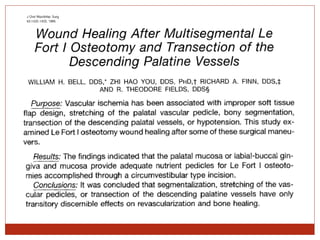
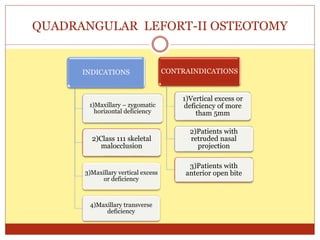
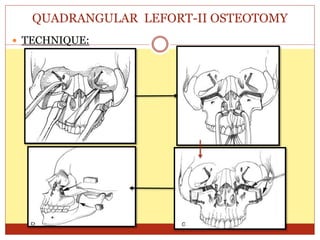
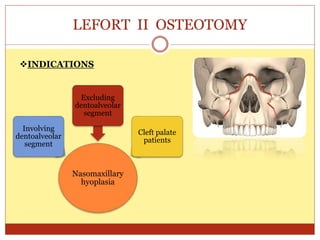
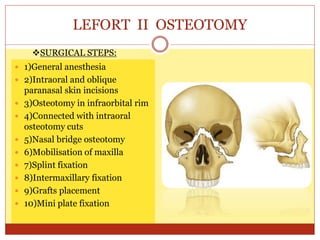
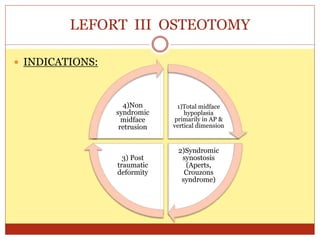
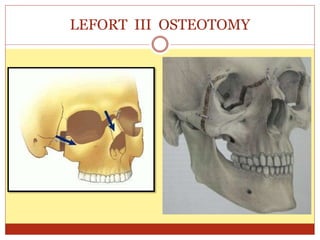
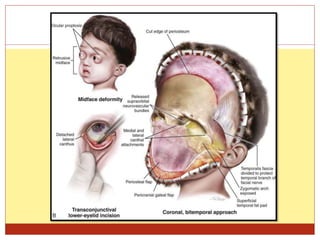
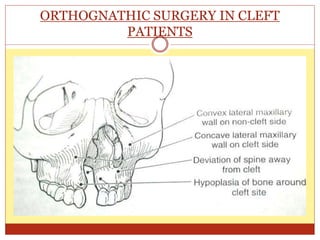
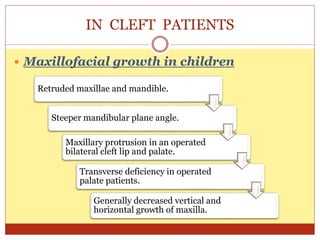
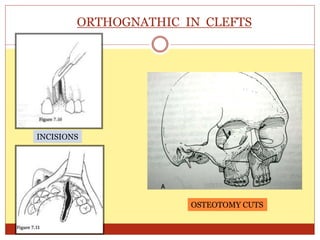
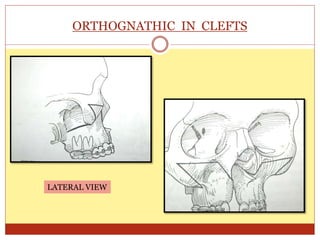
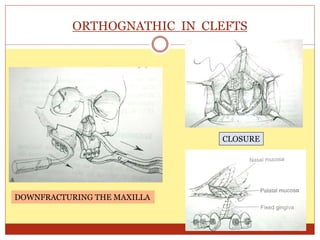
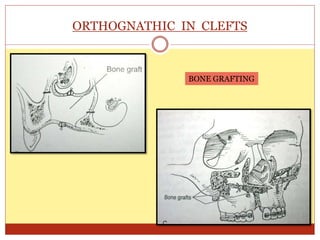
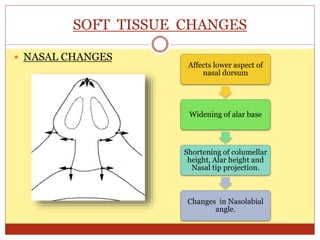
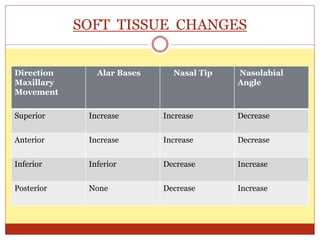
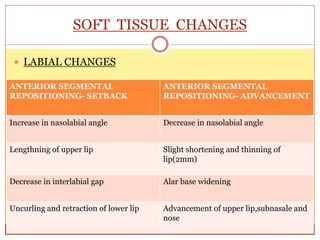
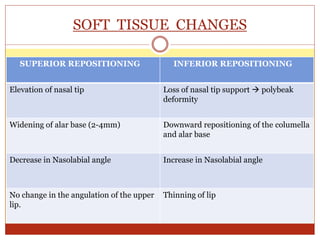
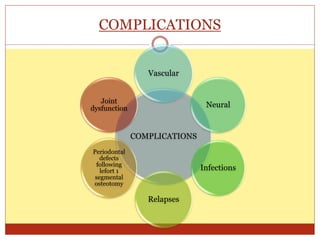
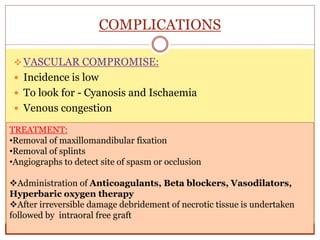
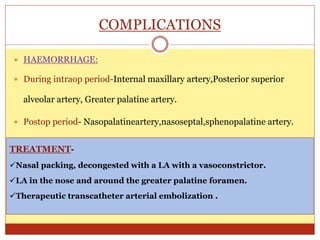
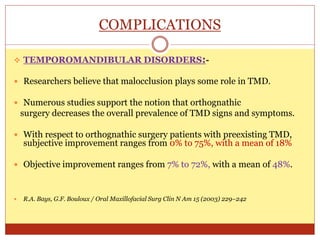
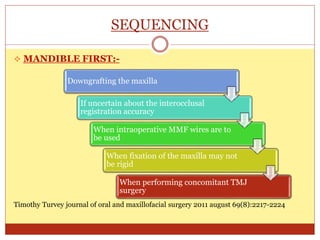
The document presents an overview of maxillary orthognathic procedures, discussing the history, anatomical considerations, various surgical techniques (like segmental and LeFort osteotomies), and soft tissue changes associated with these surgeries. It highlights the importance of addressing dentofacial deformities, which affect a significant portion of the population and can lead to functional and aesthetic issues. Complications, patient expectations, and surgical considerations are also underscored, emphasizing the need for expertise in managing such complex interventions.