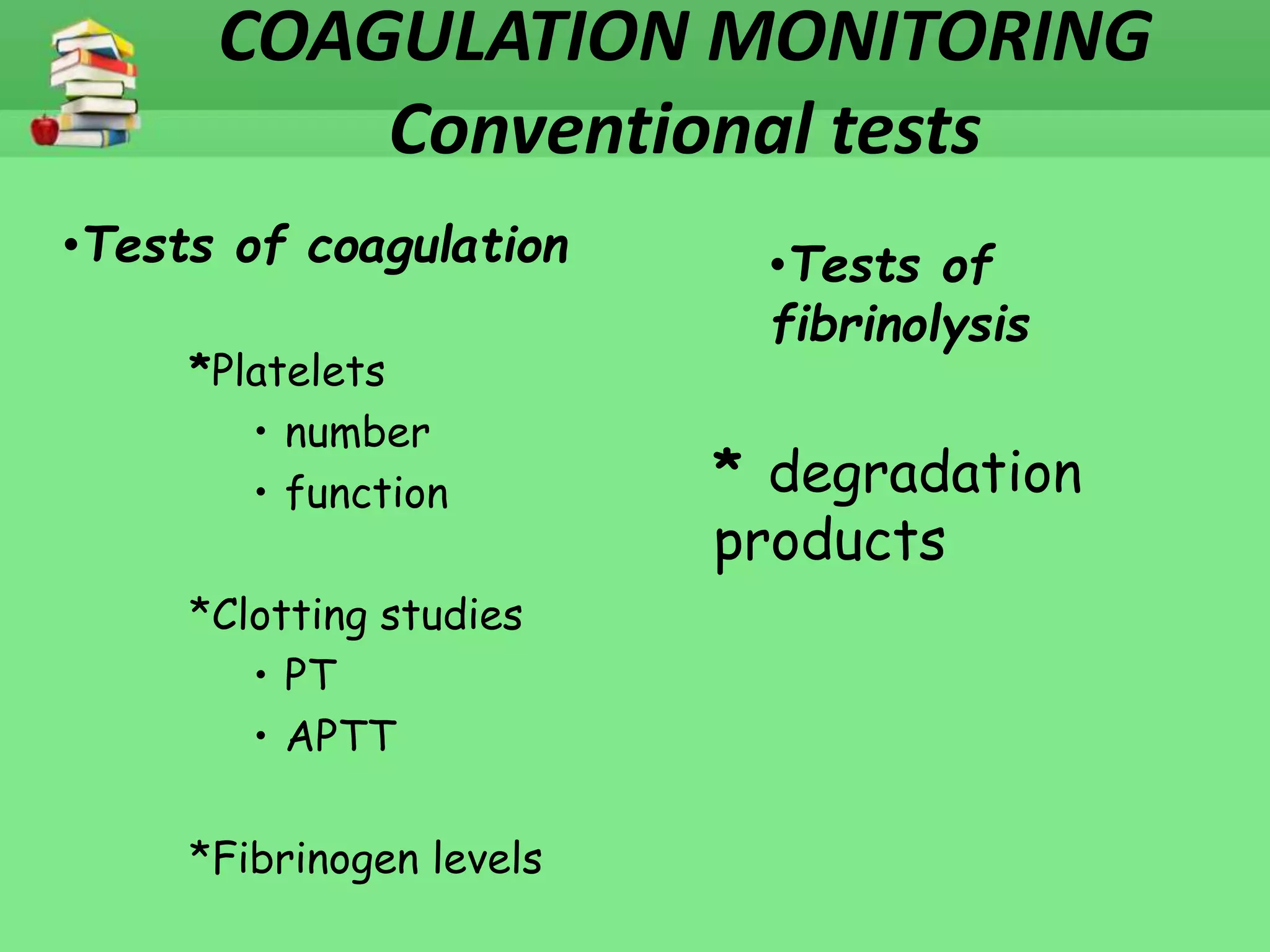
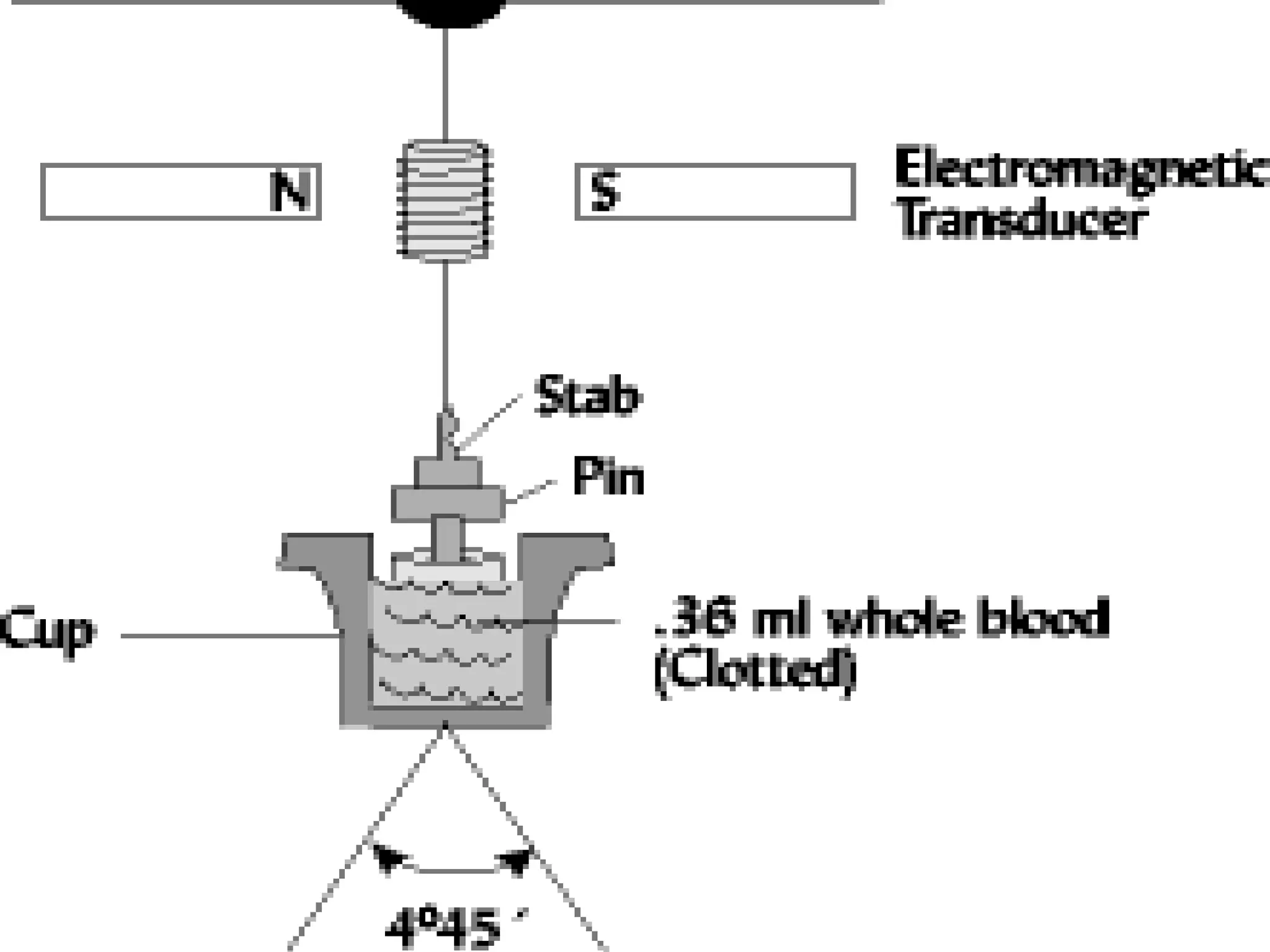
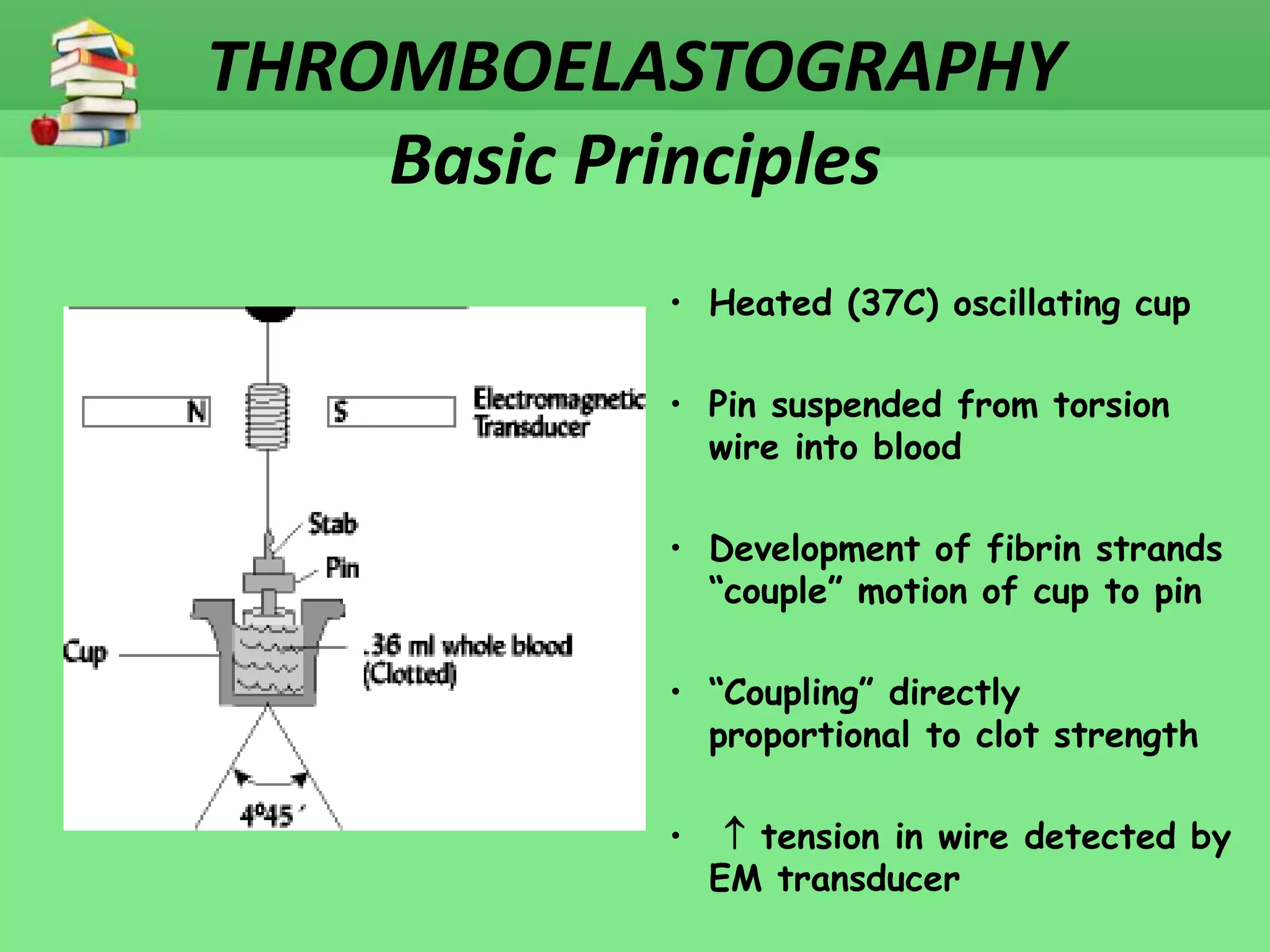
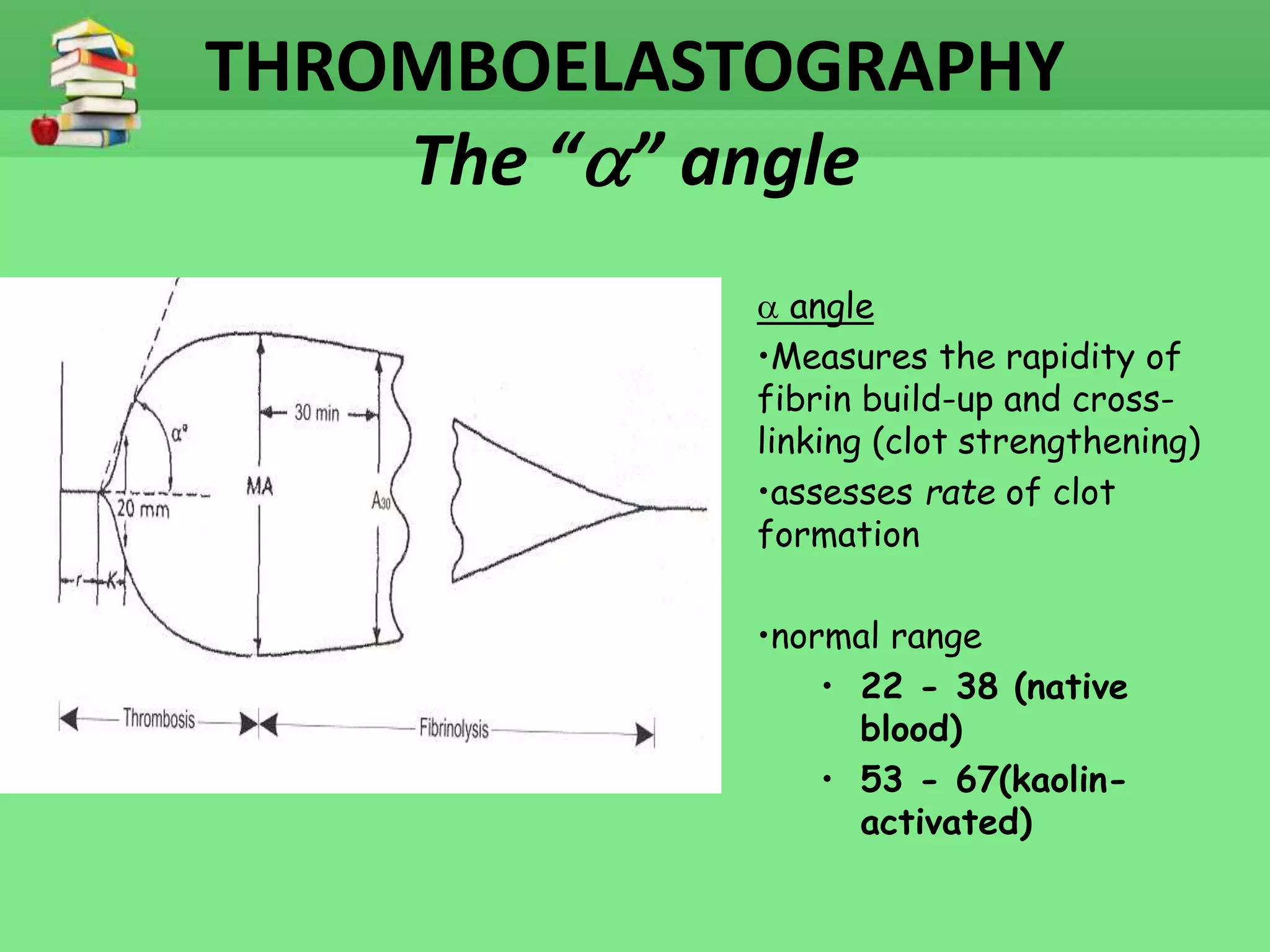
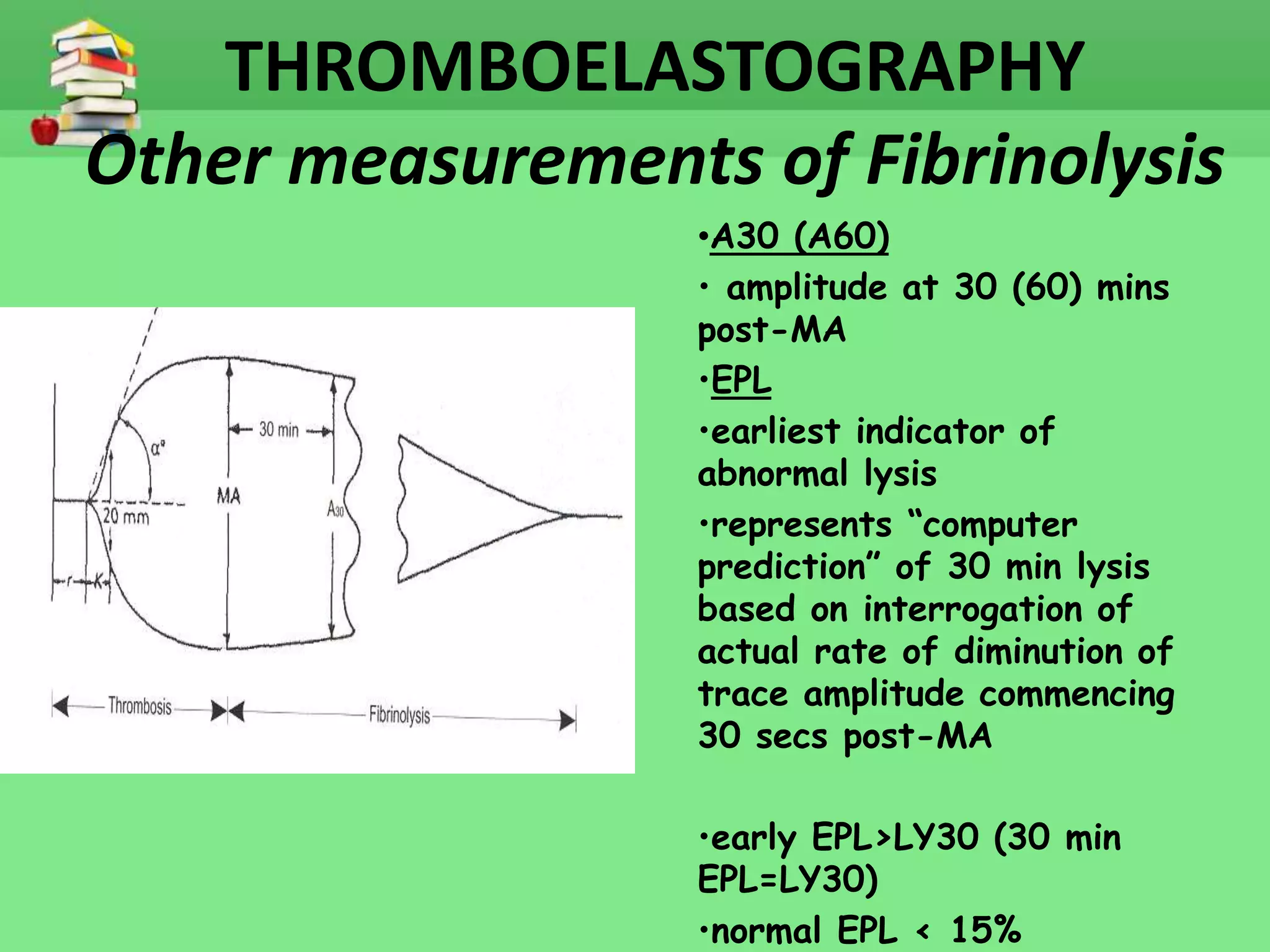
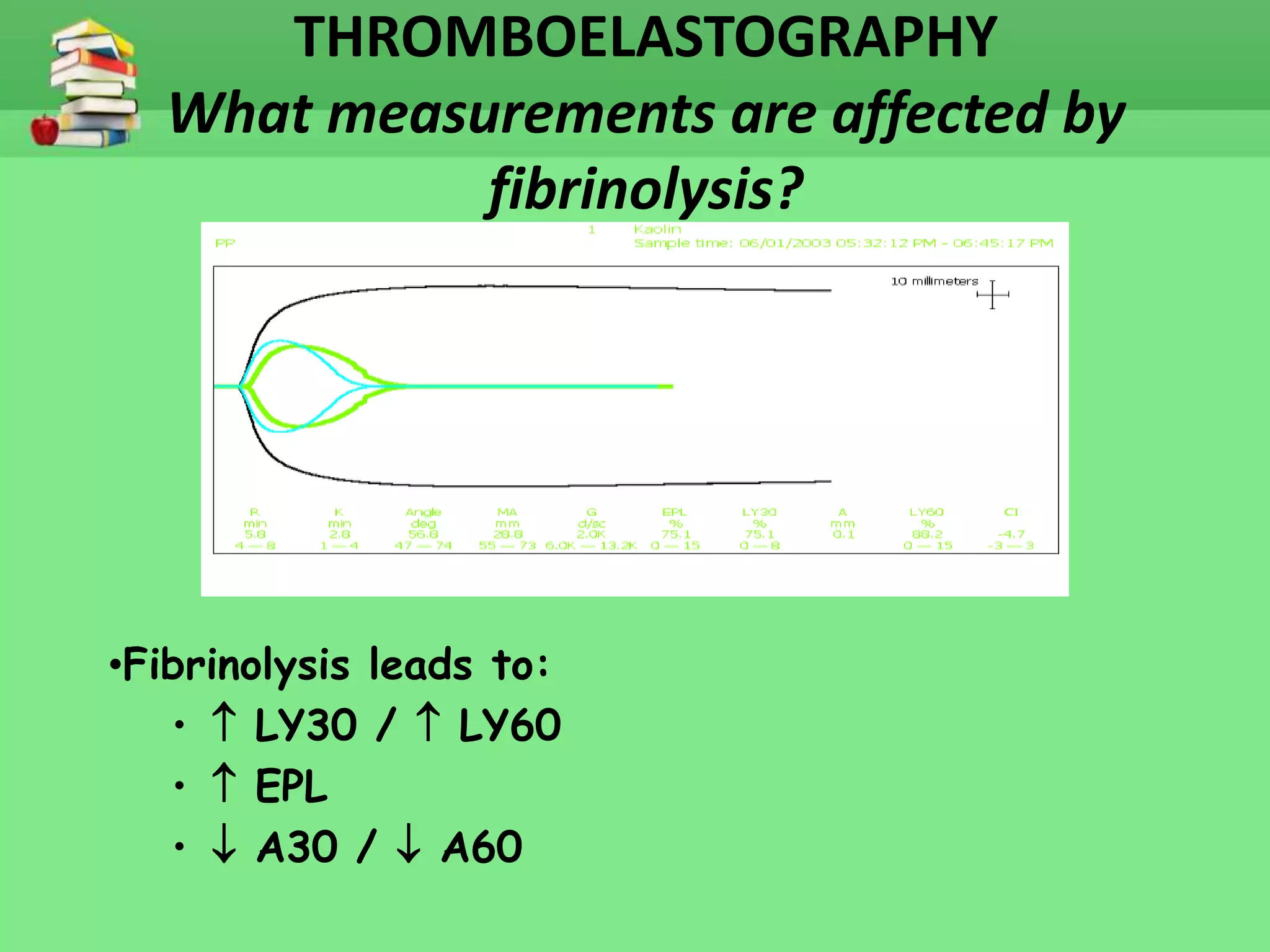
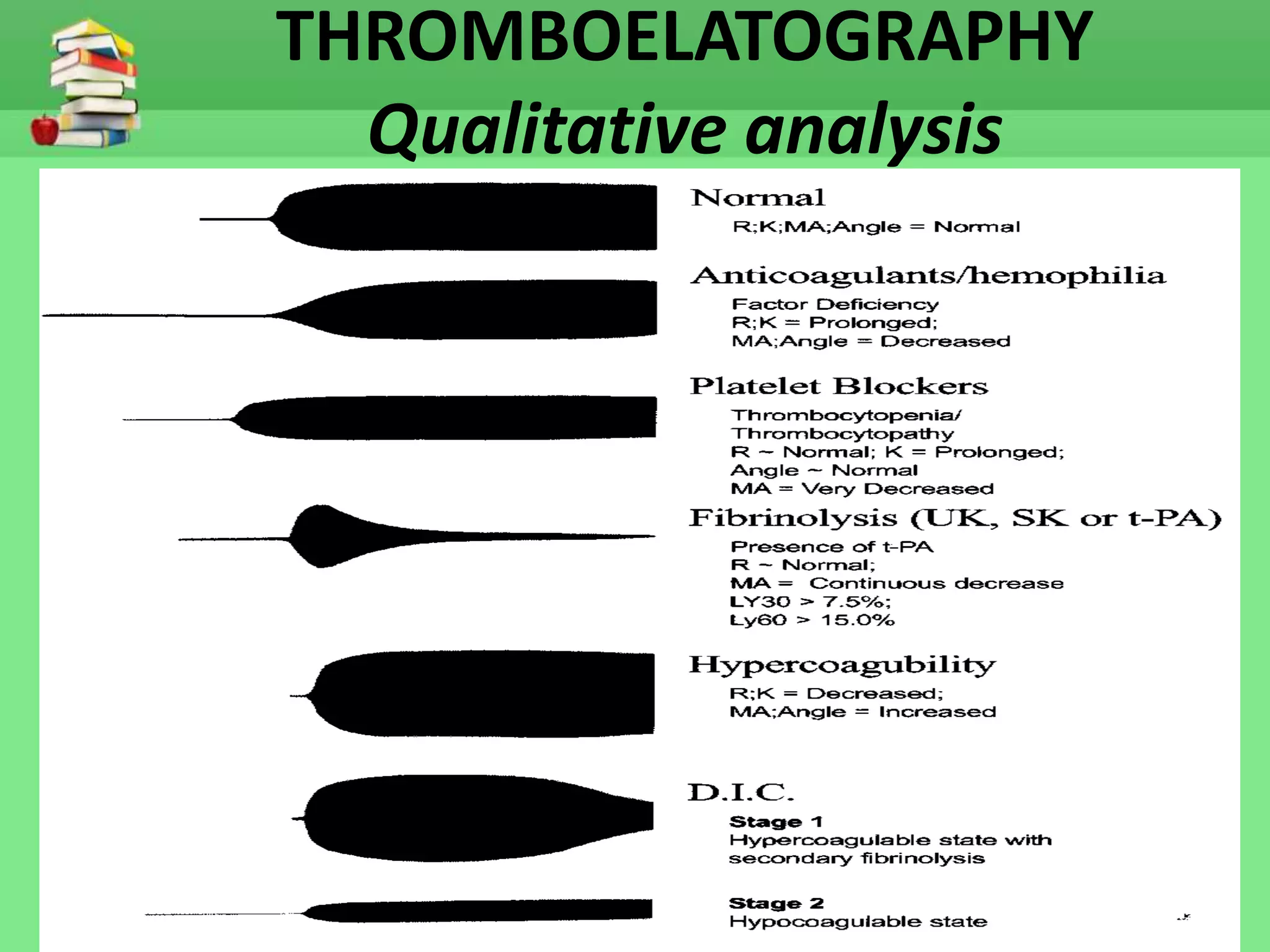
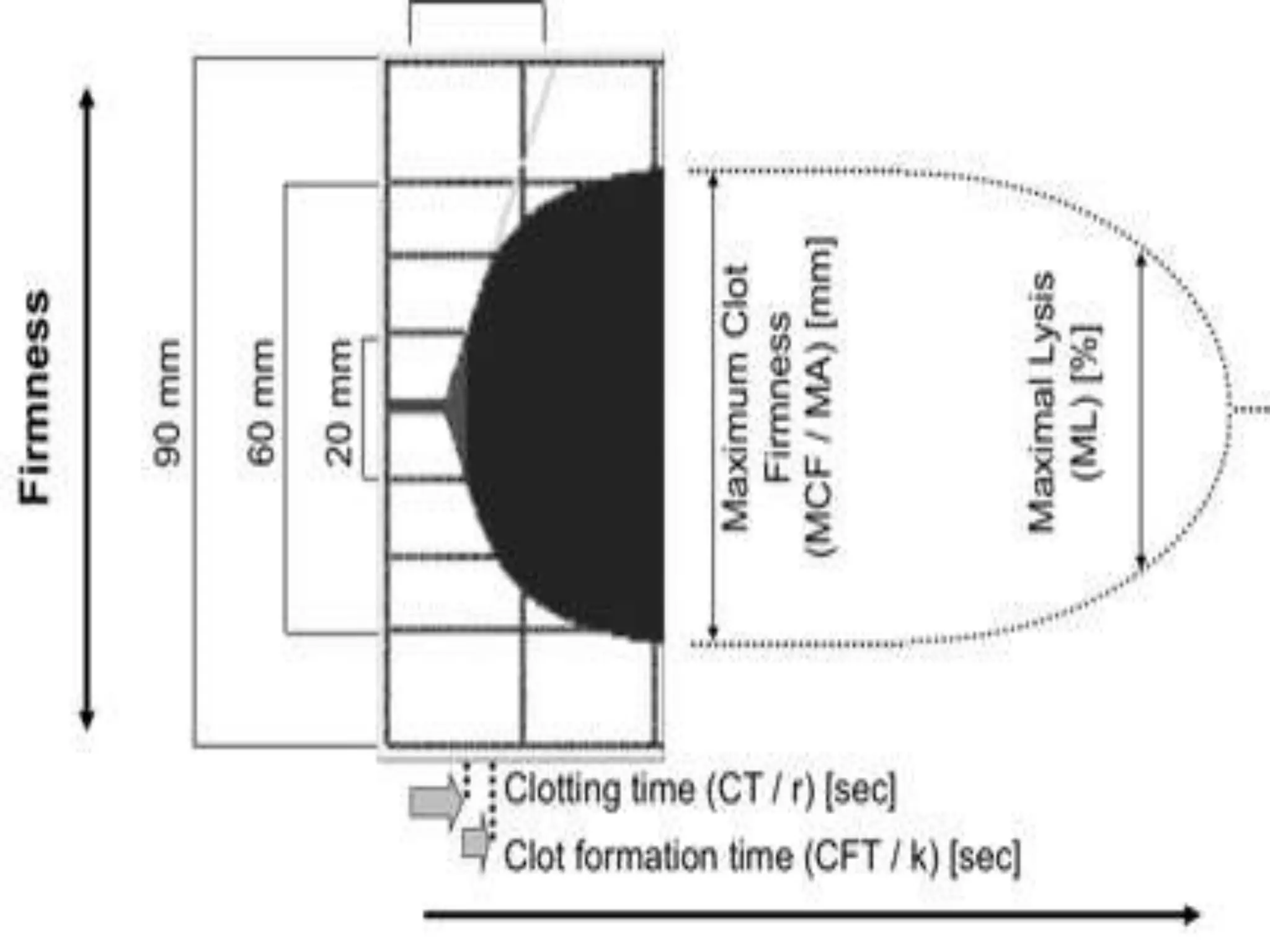
The document discusses thromboelastography (TEG), a technique for assessing whole blood coagulation. TEG monitors the viscoelastic properties of clotting blood to evaluate clot formation, kinetics, strength and stability. It provides a global assessment of hemostasis and can detect coagulation factor deficiencies, platelet issues and fibrinolysis. TEG results are rapid and help guide treatment, unlike conventional coagulation tests which examine isolated parts of the clotting process. Measurements from a TEG tracing include r and k times, alpha angle, maximum amplitude and lysis parameters. TEG gives useful qualitative and quantitative analysis of hemostasis.