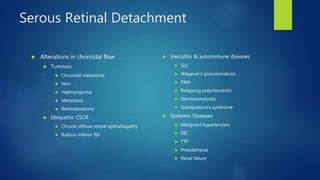
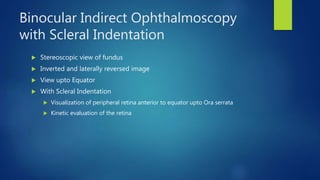
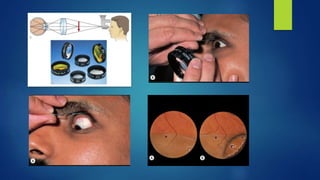
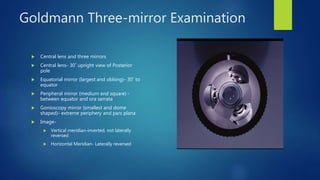
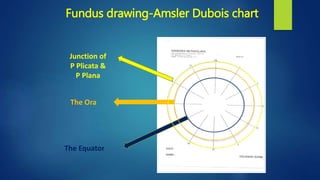
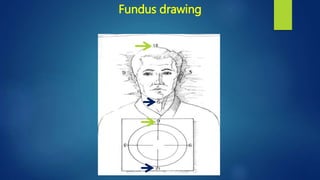
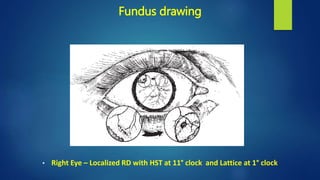
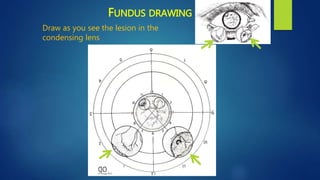
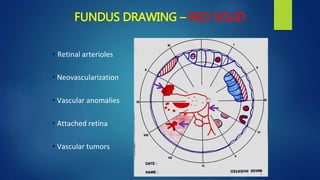
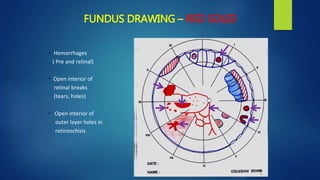
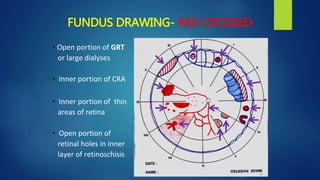
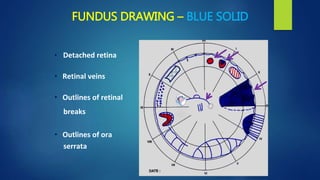
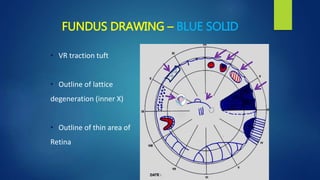
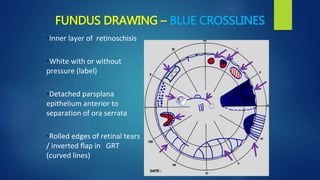
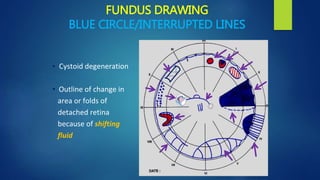
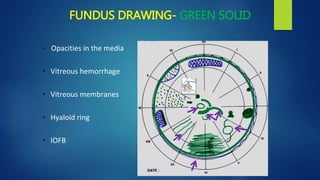
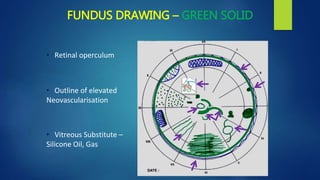
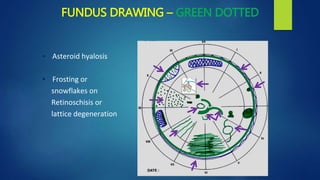
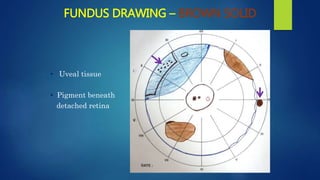
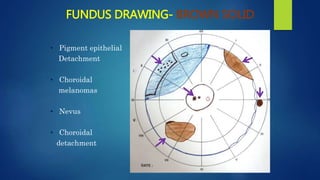
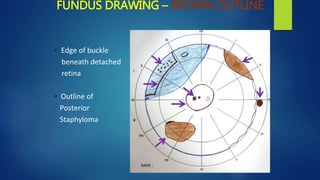
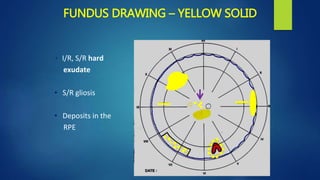
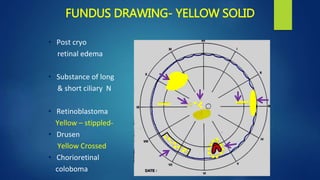
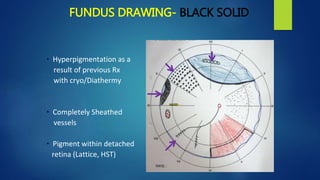
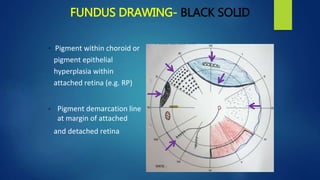
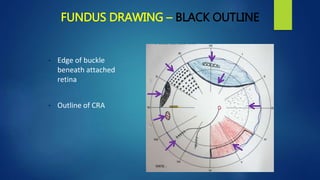
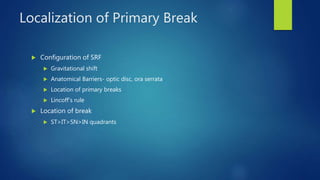
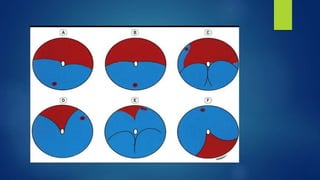
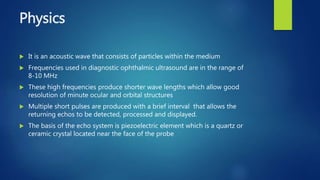
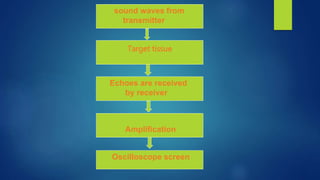
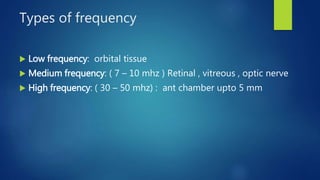
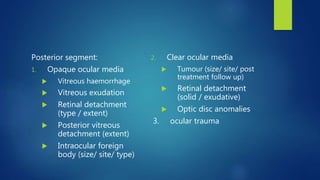
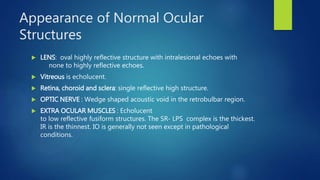
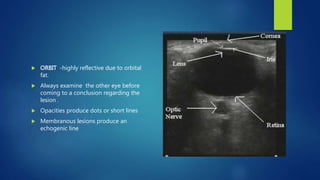
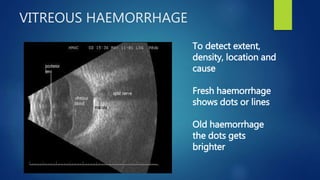
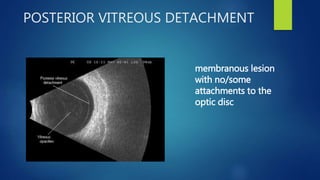
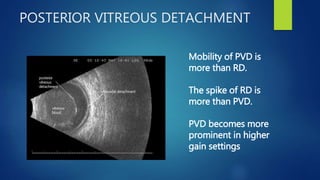
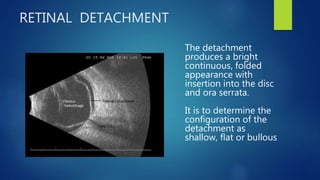
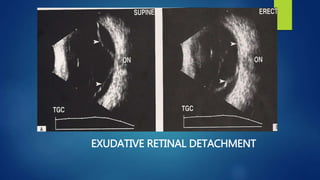
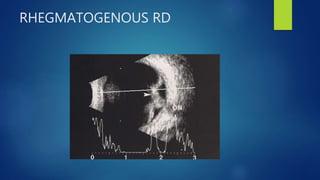
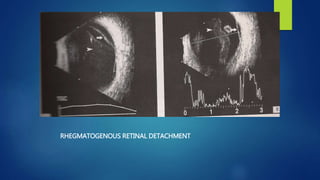
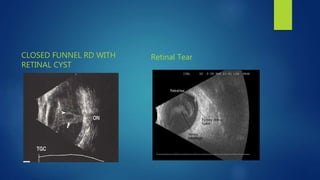
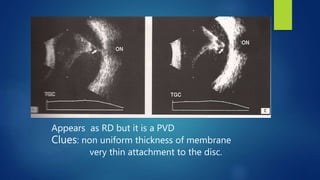
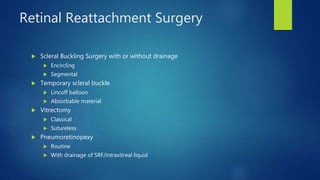
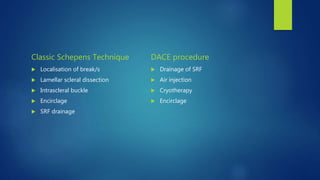
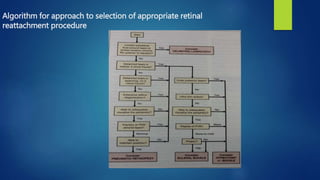
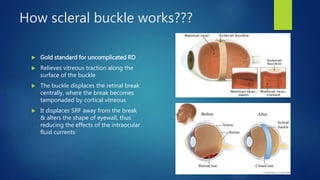
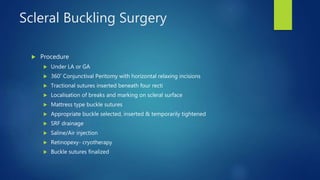
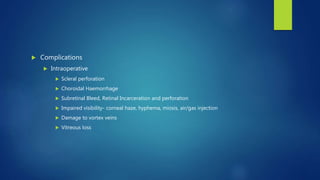
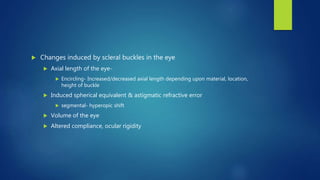
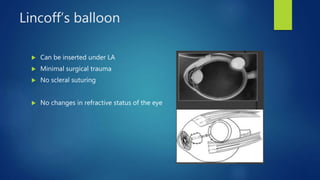
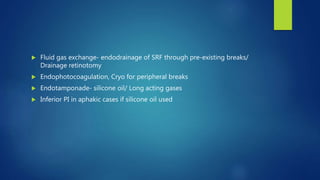
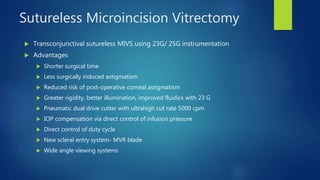
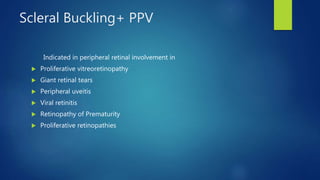
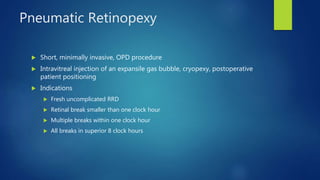
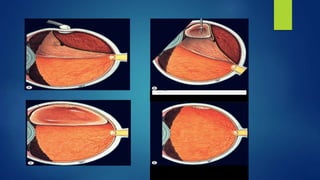
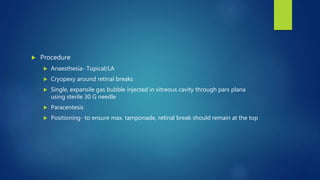
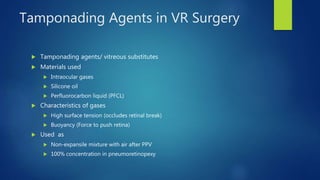
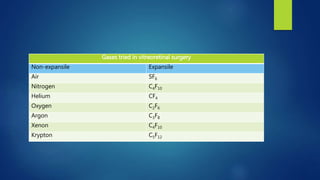
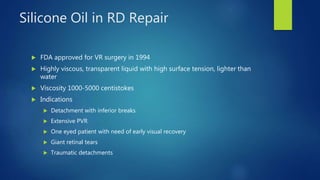
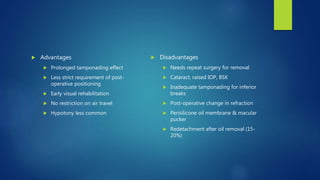
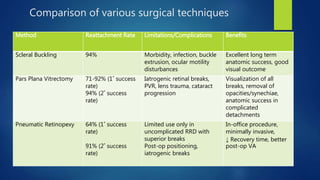
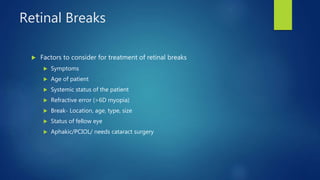
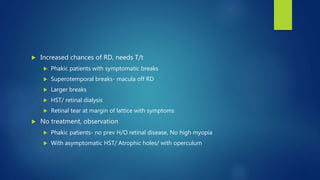
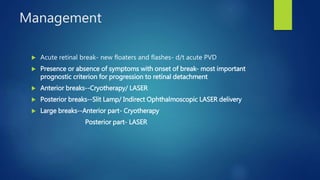
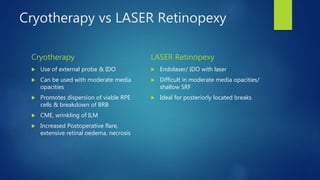
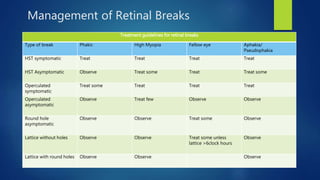
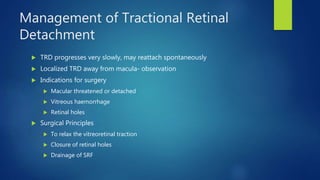
This document discusses the classification, natural history, preoperative evaluation, and management of various types of retinal detachments. It covers rhegmatogenous retinal detachment, tractional retinal detachment, exudative retinal detachment, and classifications such as primary versus secondary detachments. Preoperative evaluation includes clinical examination techniques like binocular indirect ophthalmoscopy, fundus drawing and ultrasound. Management principles and techniques like scleral buckling surgery, pneumatic retinopexy and vitrectomy are outlined.