This document discusses fluorescent angiography (FFA). It provides information on:
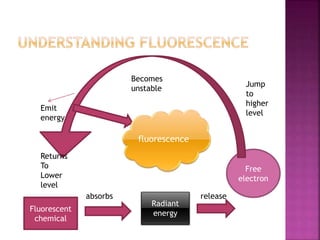
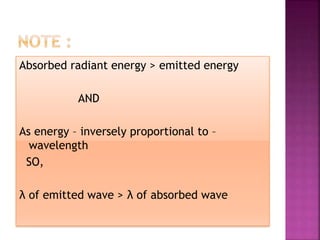
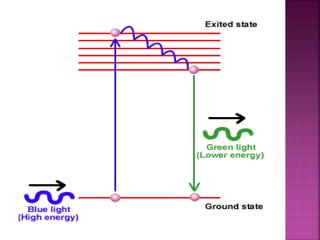
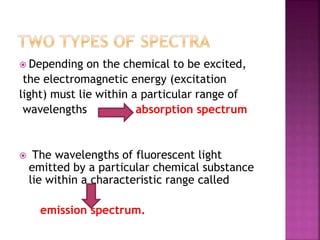
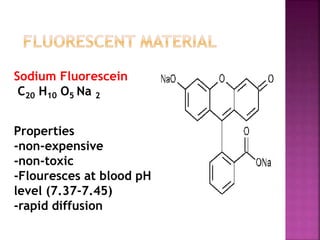
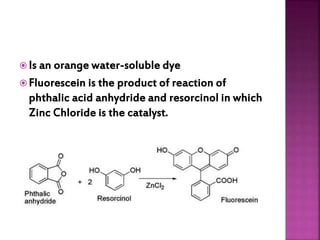
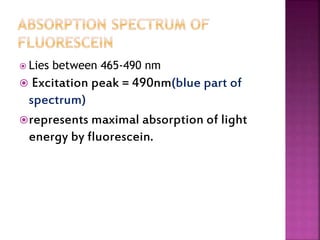
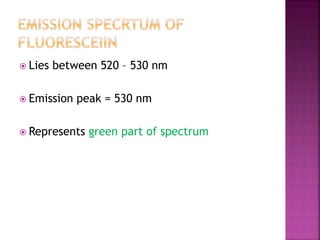
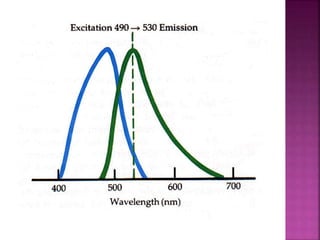
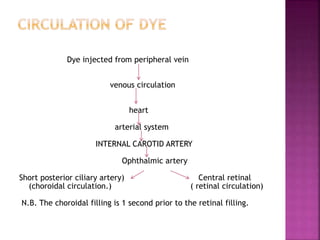
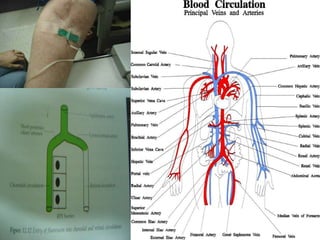
1. How fluorescent dyes like sodium fluorescein work by absorbing radiant energy and emitting light energy during fluorescence.
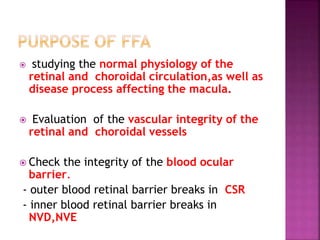
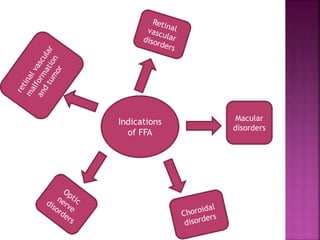
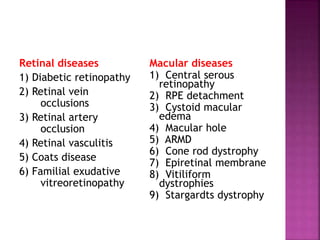
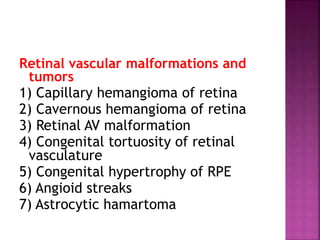
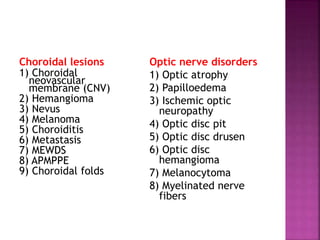
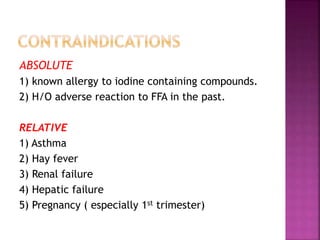
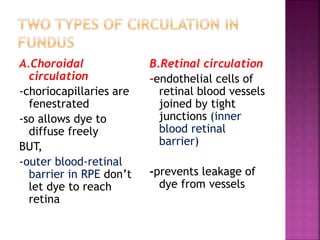
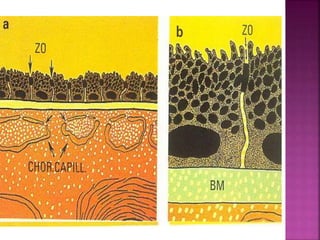
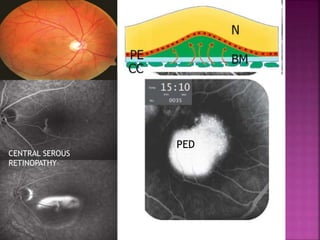
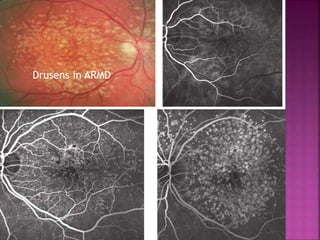
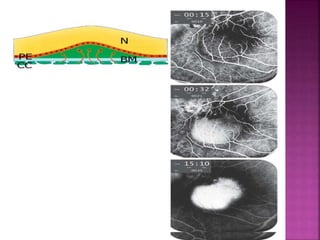
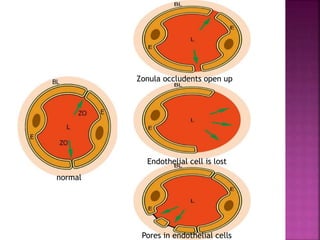
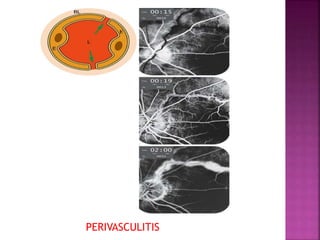
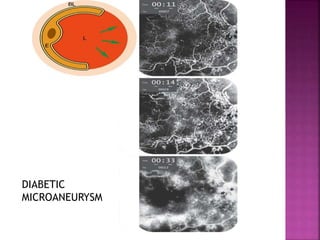
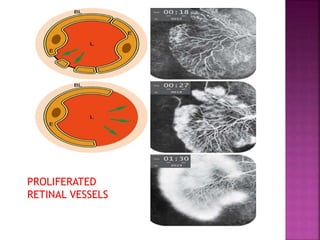
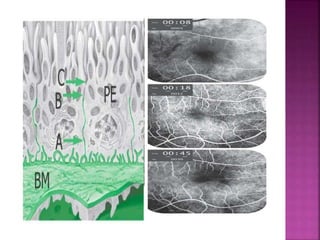
2. The uses and indications of FFA in evaluating retinal and choroidal diseases. It is used to assess vascular integrity and the blood-ocular barriers.
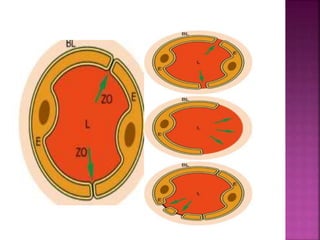
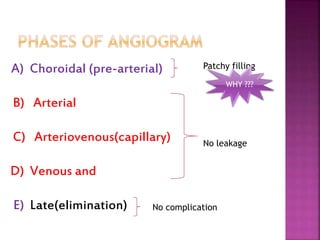
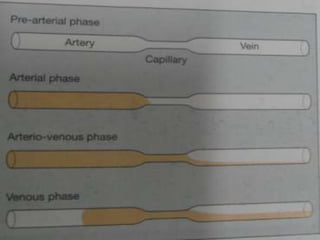
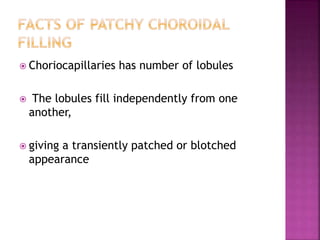
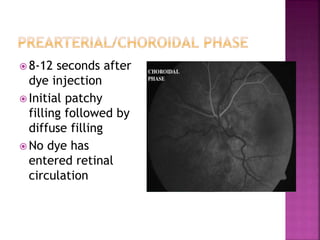
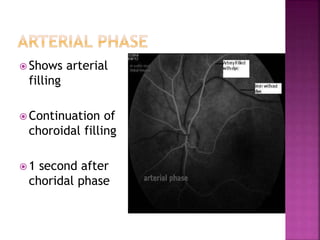
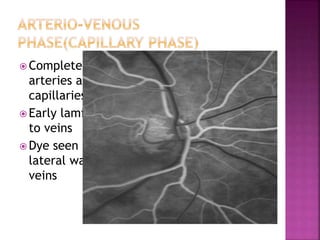
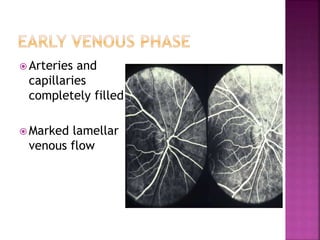
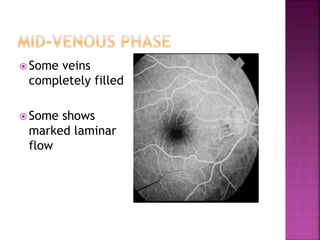
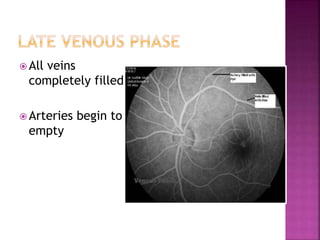
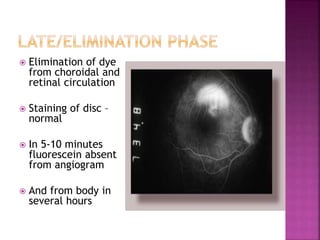
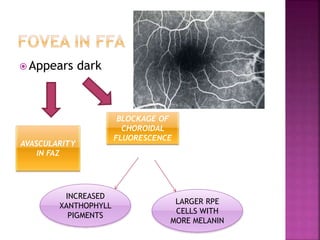
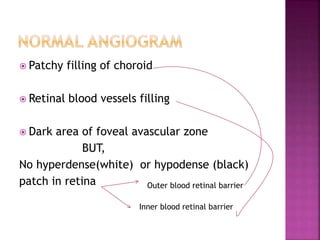
3. The phases seen during a normal FFA including the choroidal, arterial, arteriovenous, venous, and late phases.
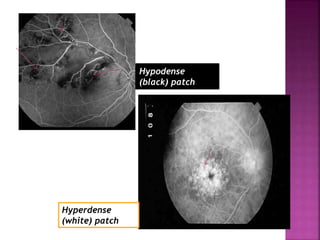
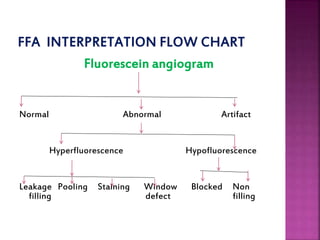
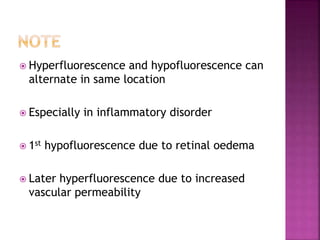
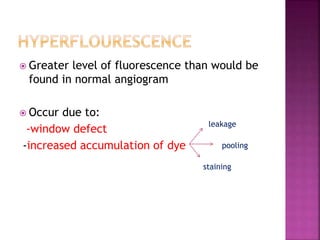
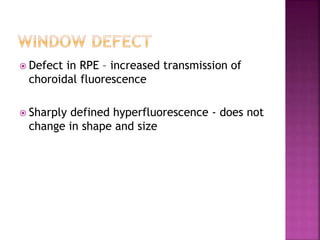
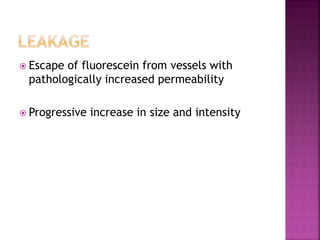
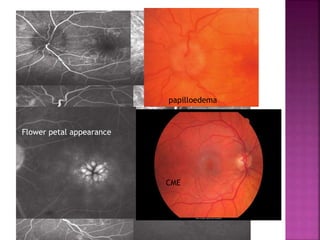
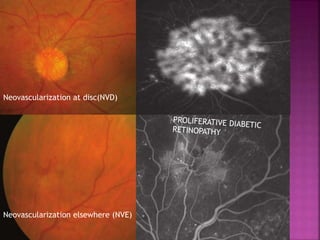
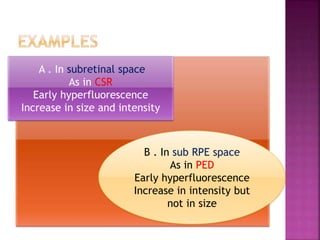
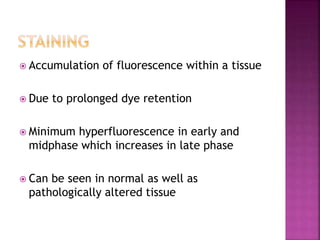
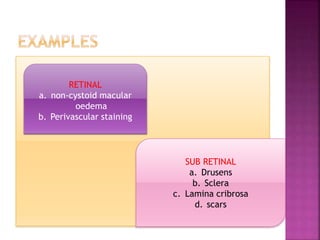
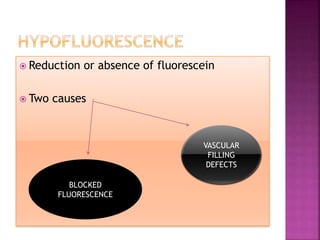
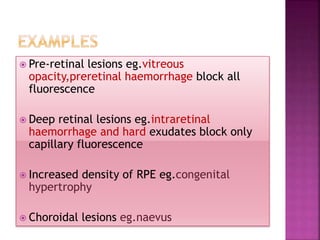
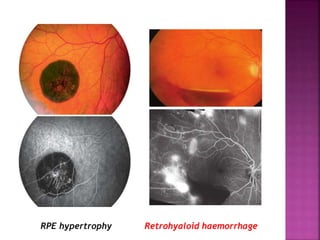
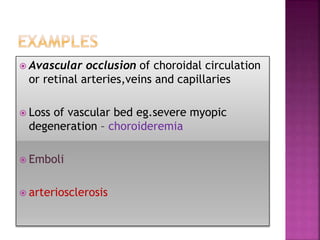
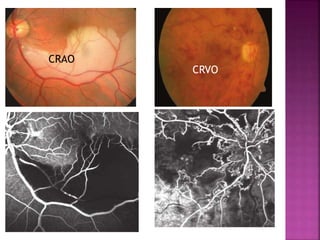
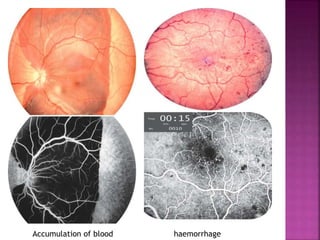
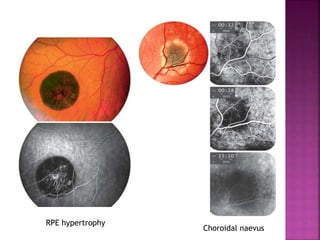
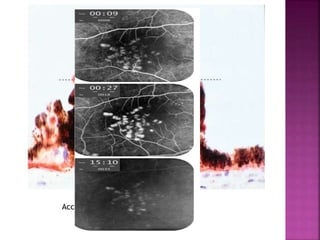
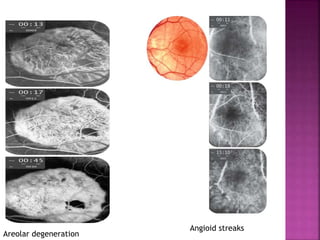
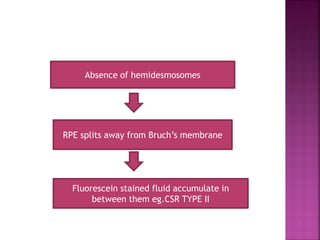
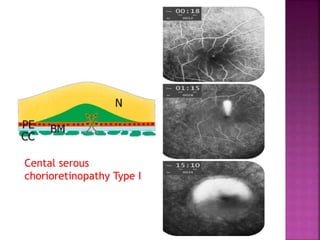
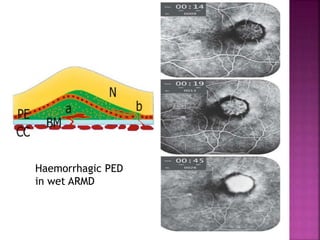
4. Common abnormalities seen on FFA including leakage, pooling, staining, hyperfluorescence, hypofluorescence, and filling defects. These provide information on disease diagnosis and monitoring.