Embed presentation
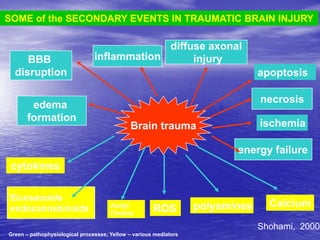

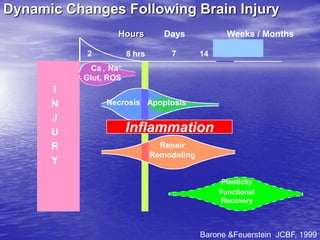
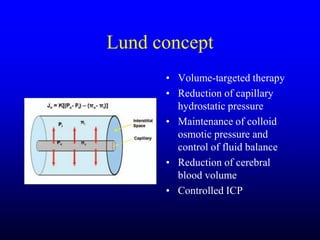
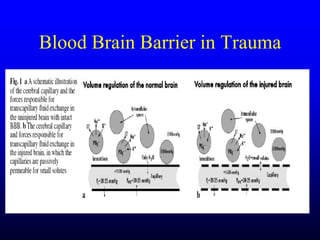
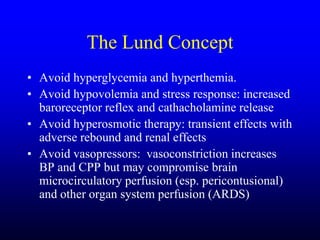
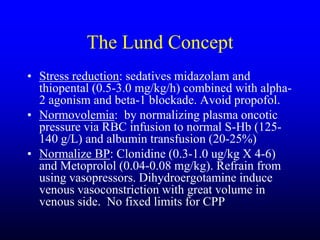
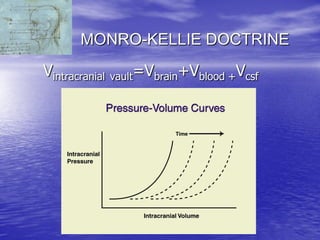
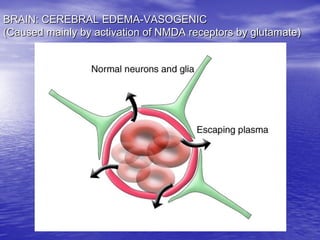
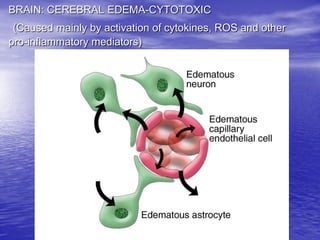
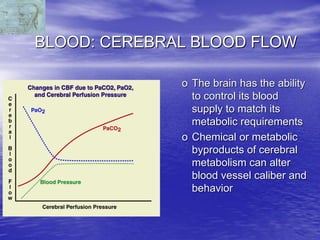
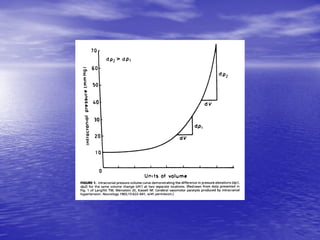

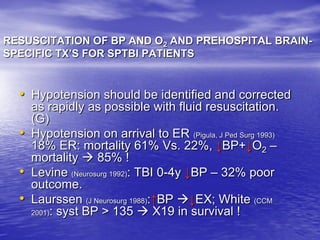
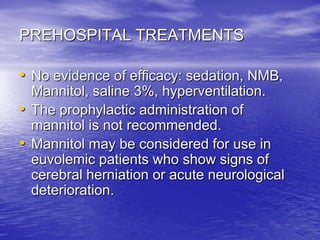
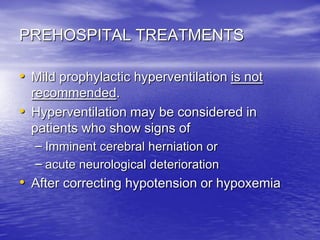
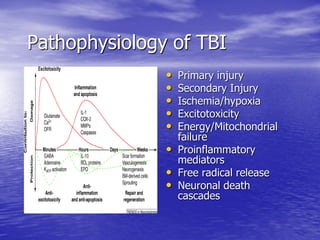
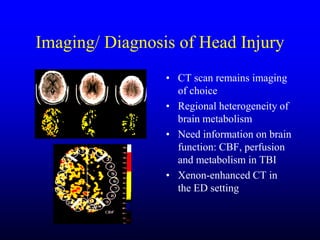
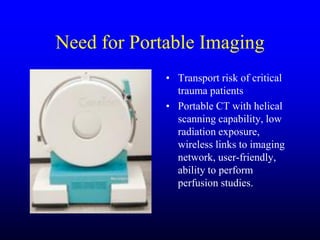
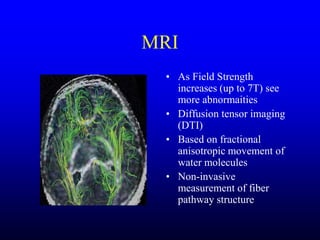
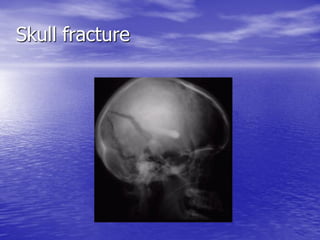
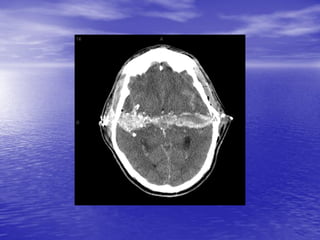
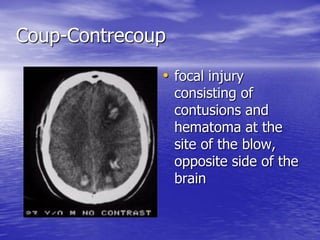
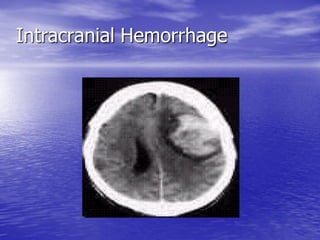
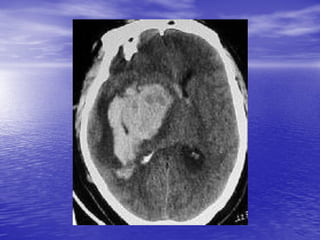
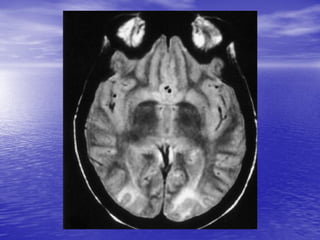
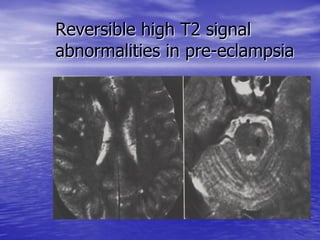
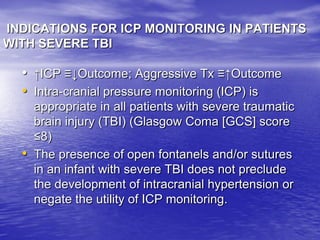
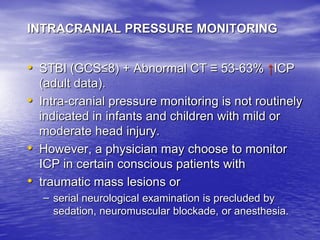
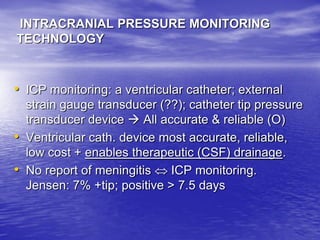
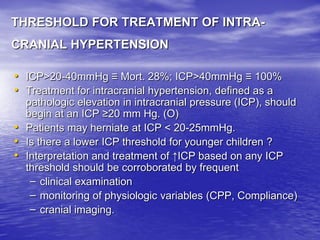
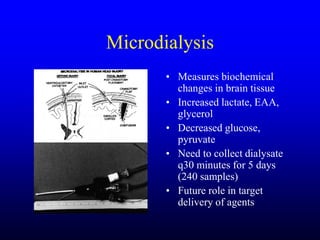
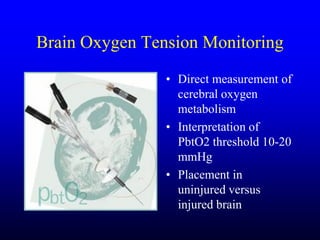
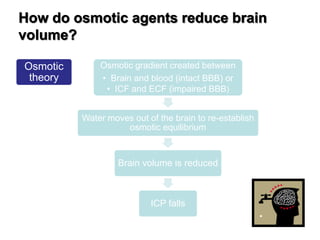
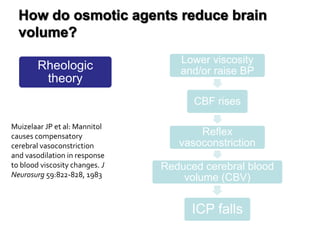
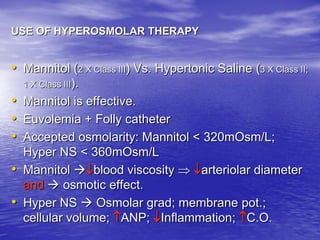
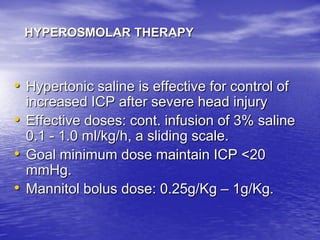
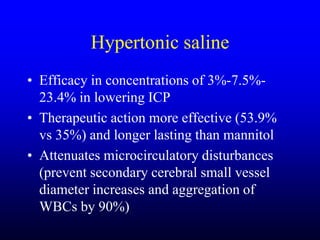
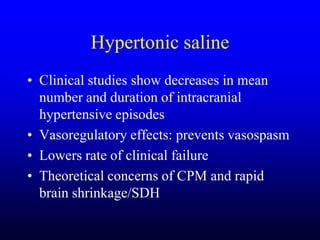
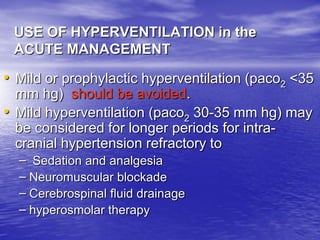
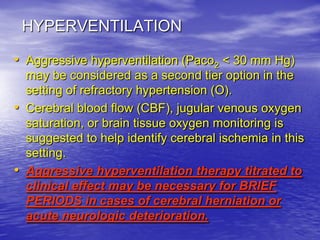
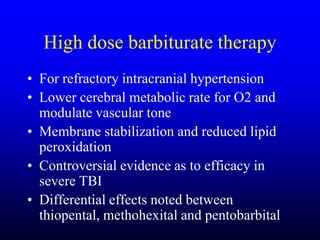
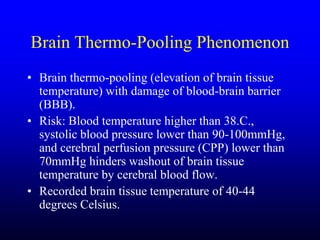
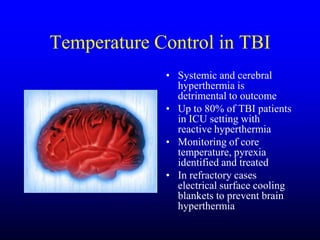


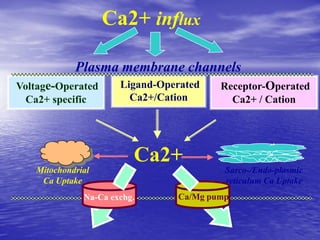

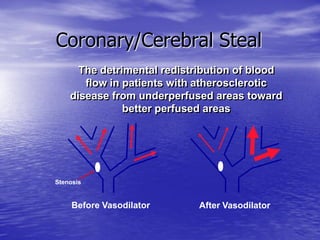



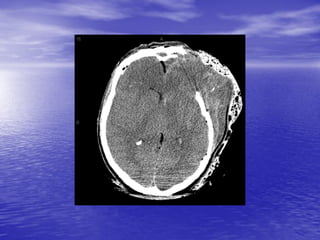
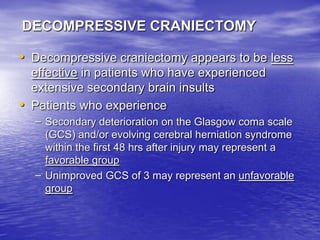

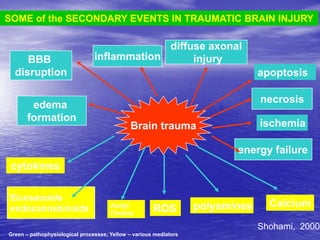
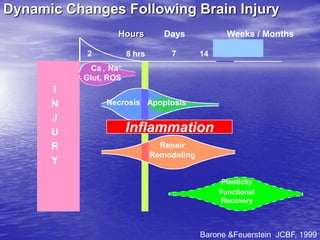
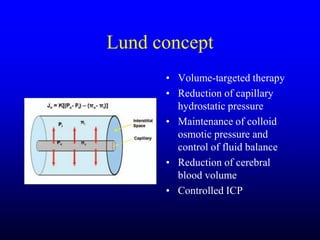
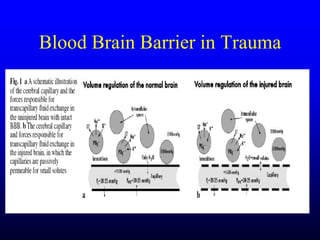
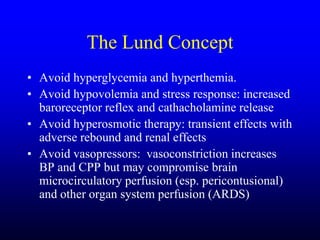
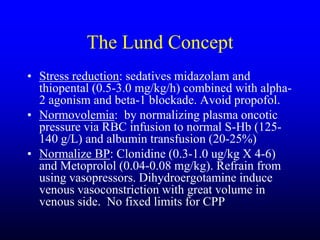
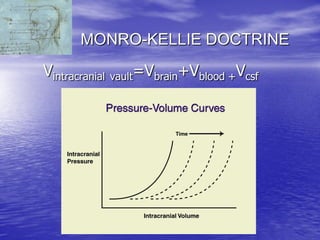
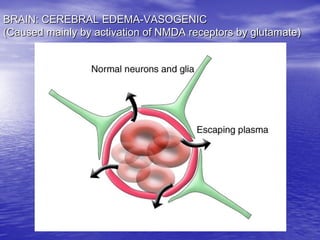
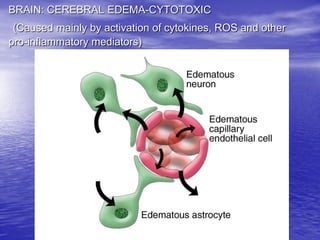
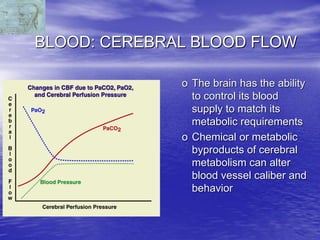
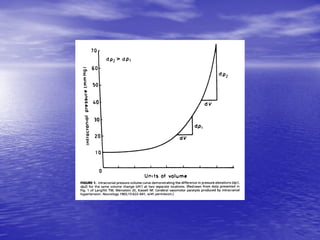
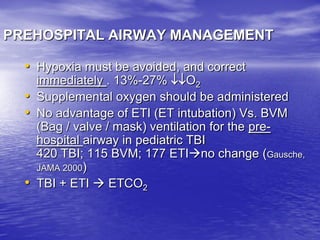
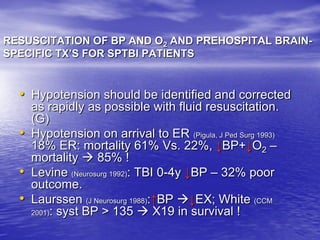
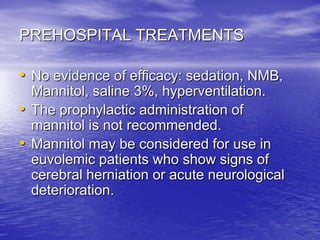
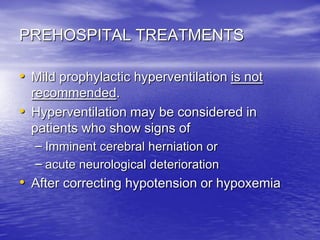
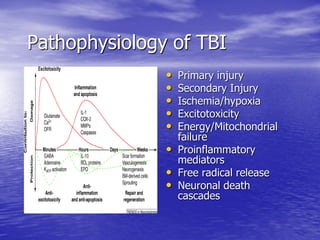
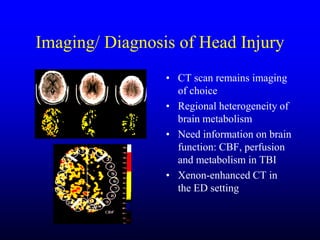
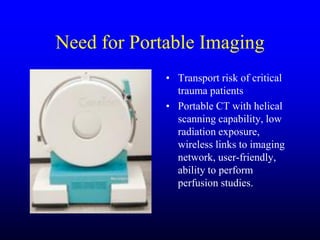
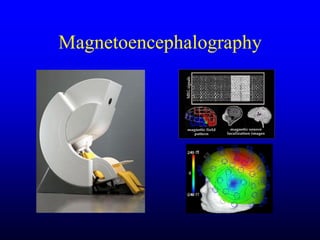
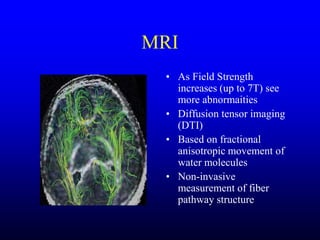
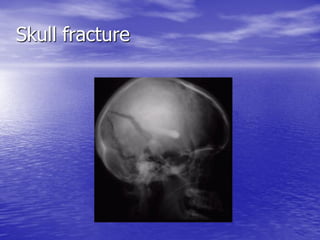
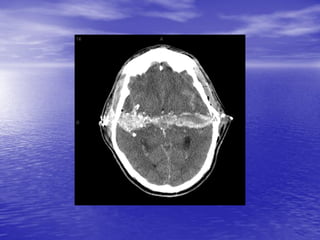
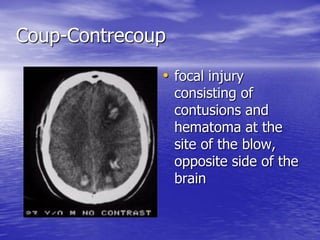
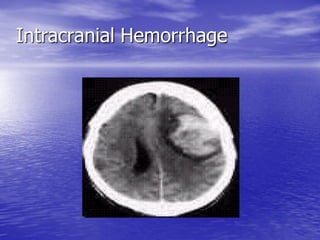
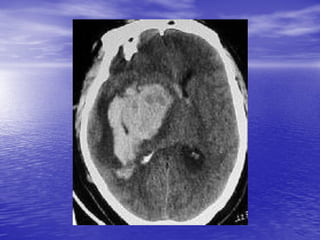
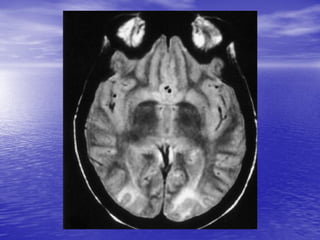
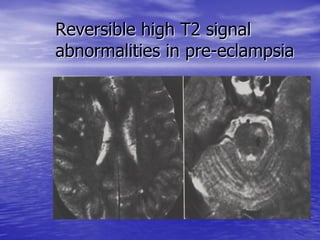
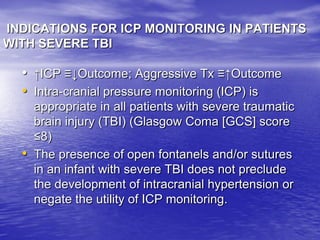
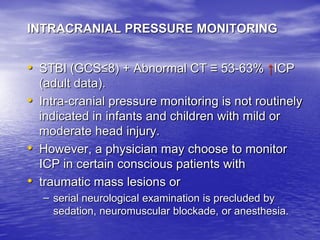
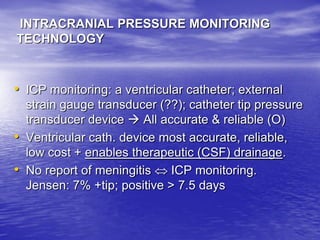
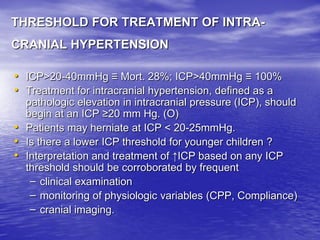
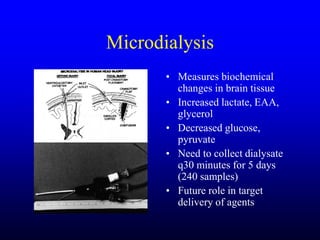
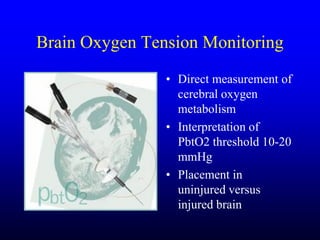
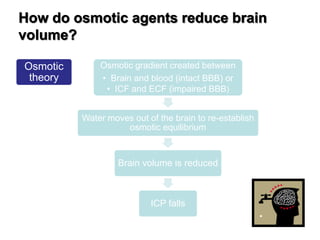
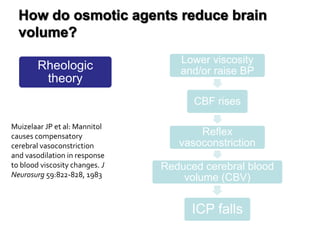
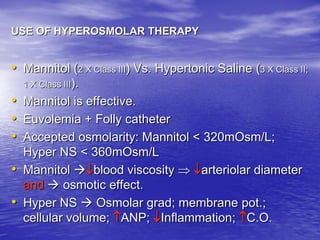
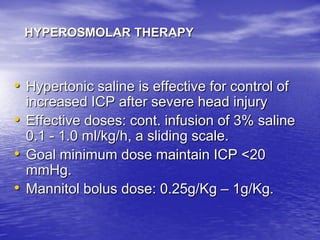
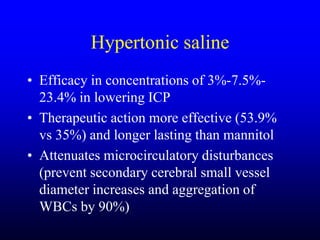
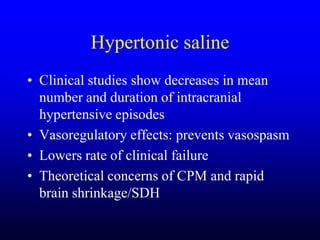
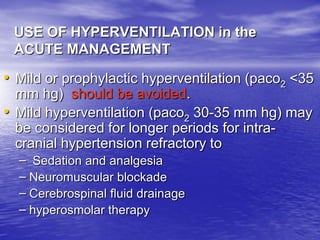
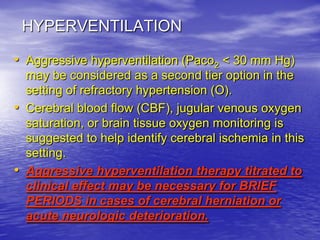
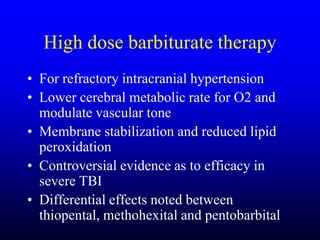
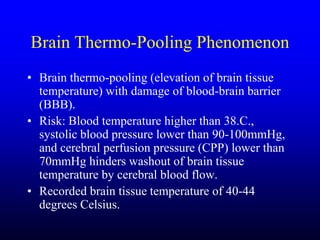
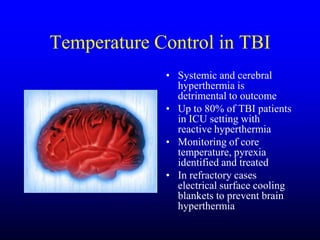
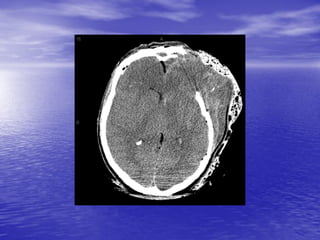
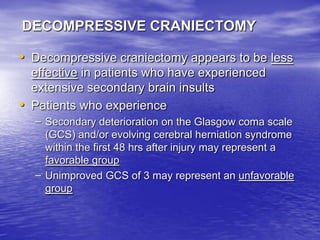
This document discusses the management of intracranial pressure and cerebral edema in neurocritical care patients. It covers topics such as how patients typically present with brain injuries, important caveats in neurological examinations, principles of cerebral resuscitation, mechanisms of primary and secondary brain injury, the pathophysiology over time, imaging techniques including CT scans and MRI, monitoring techniques like intracranial pressure monitoring, and treatment approaches like the use of hyperosmolar therapy with mannitol or hypertonic saline. The goal is to prevent secondary brain injury after the initial primary injury occurs.