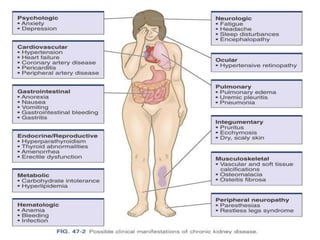
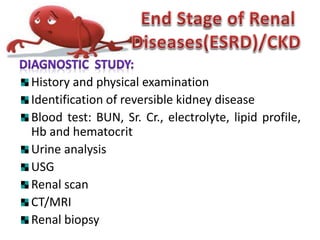
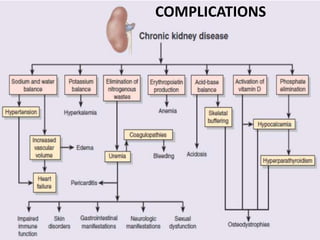
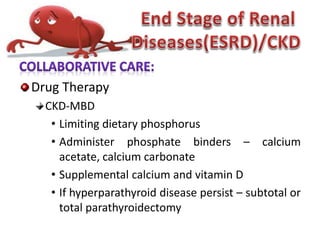
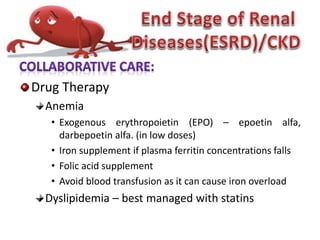
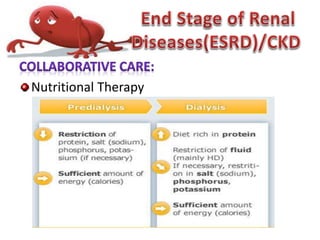
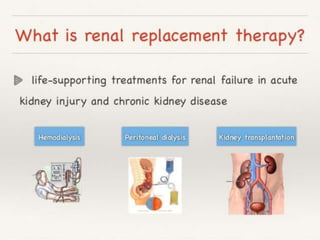
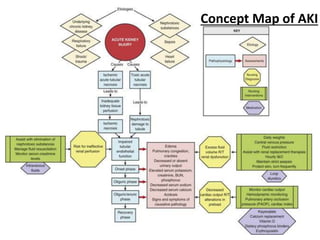
The document discusses acute renal failure (also known as acute kidney injury) and chronic kidney disease (CKD), detailing their causes, symptoms, and treatment options. It describes acute kidney injury as a sudden decline in kidney function due to prerenal, intrarenal, or postrenal factors, while chronic kidney disease is a progressive and irreversible loss of kidney function due to conditions like diabetes and hypertension. Various treatment strategies, including medication, dietary management, and renal replacement therapy, are highlighted to manage these kidney disorders.
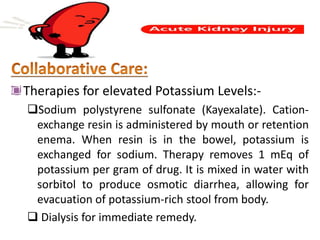
![IV fluids if the renal failure is due to fluid loss.
Diuretics is often administered but not
recommended in high doses. Loop diuretics
(furosemide [Lasix], bumetanide [Bumex]) or an
osmotic diuretic (mannitol).
If AKI is already established, forcing fluids and
diuretics will not be effective and may, in fact, be
harmful.](https://image.slidesharecdn.com/notesonrenalfailure-180514062330/85/Notes-on-renal-failure-25-320.jpg)
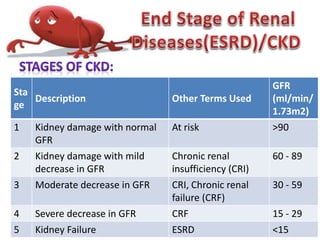
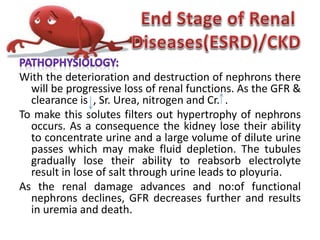
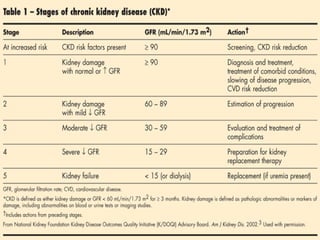
![Patients with chronic kidney disease (CKD) stages 1-
3 (glomerular filtration rate [GFR] >30
mL/min/1.73 m²) are frequently asymptomatic.
When the glomerular filtration rate (GFR) slows to
below 30 mL/min, signs of uremia (high blood
level of protein by-products, such as urea) may
become noticeable. When the GFR falls below 15
mL/min most people become increasingly
symptomatic.](https://image.slidesharecdn.com/notesonrenalfailure-180514062330/85/Notes-on-renal-failure-44-320.jpg)