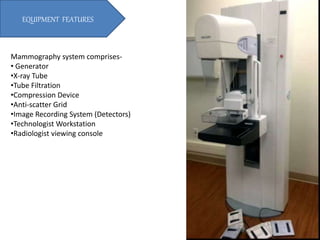
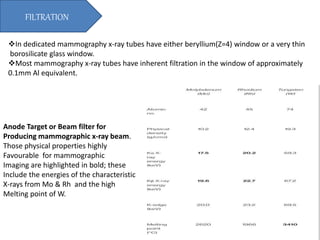
The document provides a comprehensive overview of mammography, detailing its purpose, principles, and advanced techniques such as tomosynthesis, which produces 2D and 3D breast images using low-energy x-rays. It outlines essential equipment features, imaging needs, and various components of mammography systems, emphasizing the importance of resolution, dose management, and the use of grids for improved image quality. Additionally, the document compares indirect and direct conversion methods for image detectors, highlighting their efficiency and resolution capabilities.