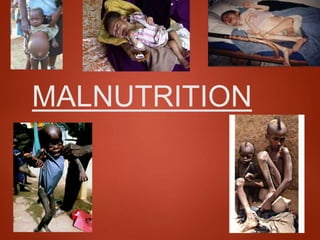
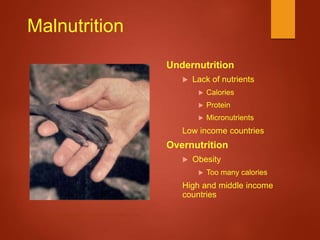
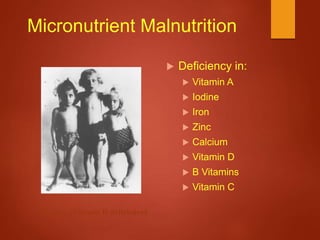
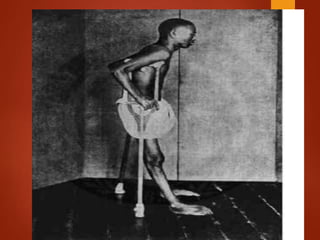
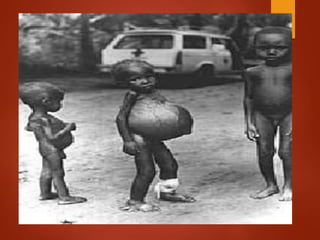
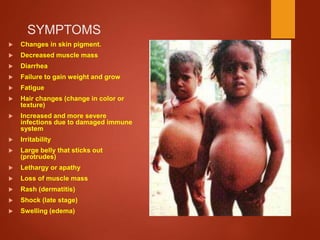
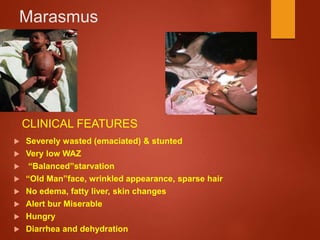
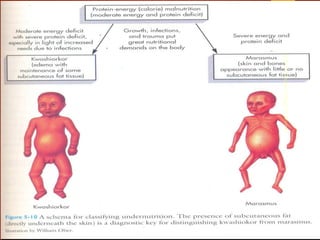
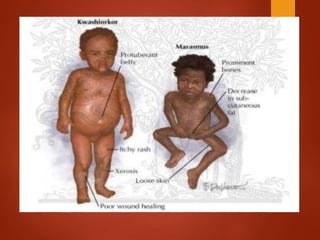
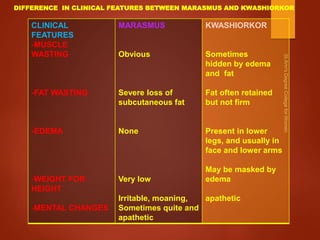
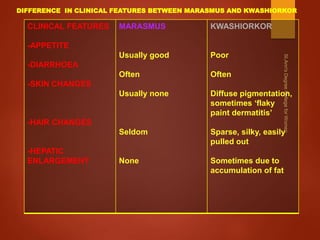
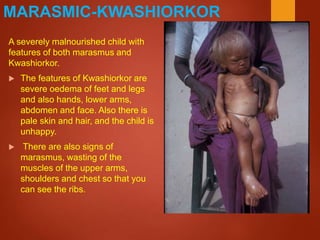
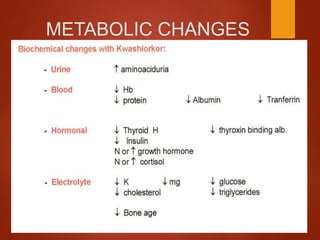
Malnutrition refers to deficiencies or excesses of nutrients that can harm health. It includes undernutrition and overnutrition. Undernutrition is caused by insufficient food intake or poor absorption of nutrients and can result in conditions like marasmus, kwashiorkor, and micronutrient deficiencies. Marasmus is characterized by wasting of muscle and tissue due to lack of calories, while kwashiorkor involves protein deficiency and swelling. Poverty is a leading cause of malnutrition globally as it limits access to nutritious foods. Treatment involves correcting nutritional imbalances through diet and supplements.