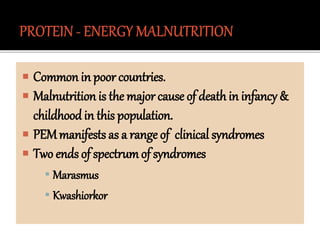
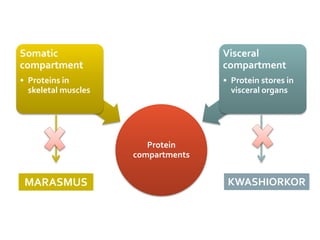
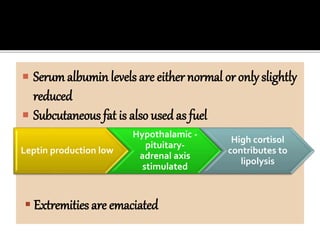
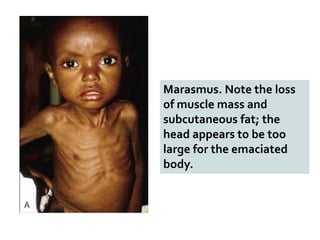
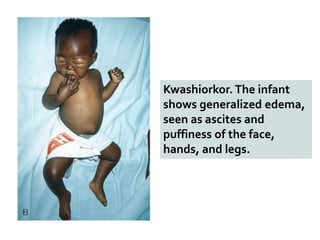
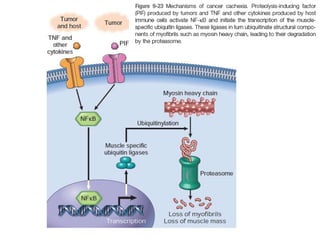
This document discusses different types of malnutrition including primary and secondary malnutrition. It describes the clinical syndromes of marasmus and kwashiorkor that represent the two extremes of protein-energy malnutrition (PEM). Marasmus is characterized by loss of muscle and fat mass while kwashiorkor presents with edema and skin changes. Anorexia nervosa, bulimia, cachexia and starvation are also summarized as forms of self-induced malnutrition.