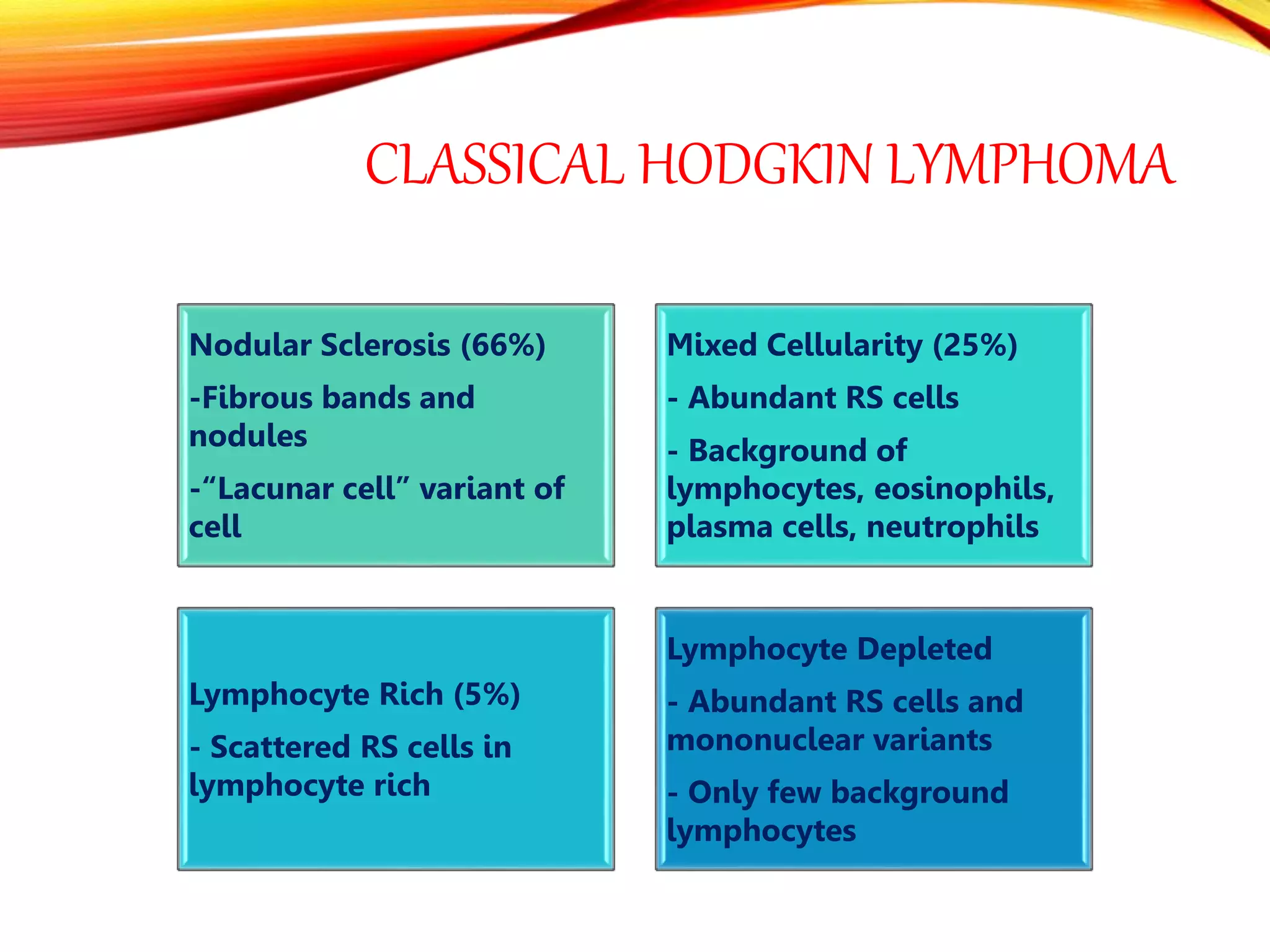
This document provides an overview of the lymphatic system and lymphadenopathy. It discusses the primary and secondary lymphoid organs, causes of lymphadenopathy including infections, immune diseases, and malignancies. Hodgkin's lymphoma and non-Hodgkin's lymphoma are described as neoplastic proliferations of white blood cells that can cause generalized lymphadenopathy. The classification, clinical features, etiology, diagnosis, and prognosis of Hodgkin's and non-Hodgkin's lymphoma are summarized. Causes of splenomegaly including infections, hematologic malignancies, and connective tissue diseases are also reviewed.