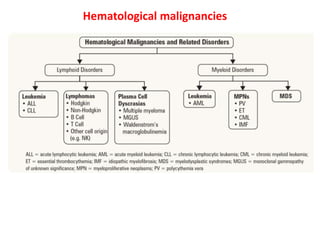
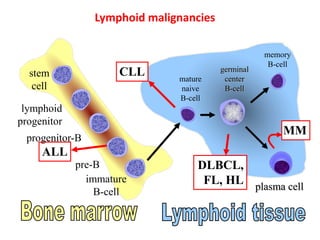
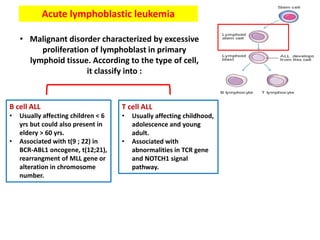
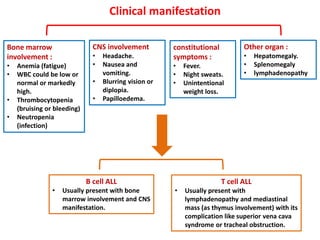
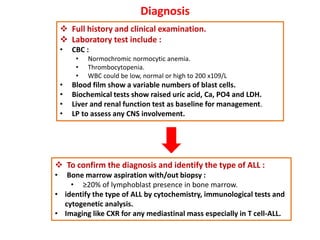
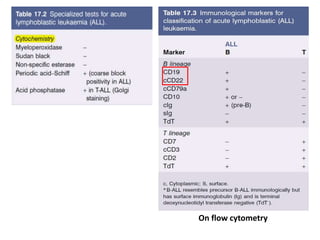
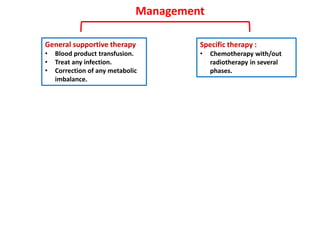
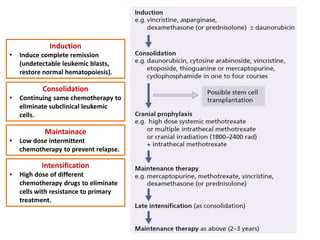
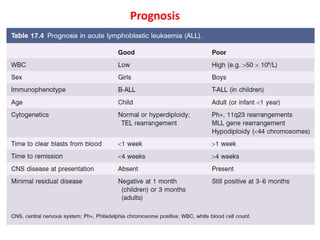
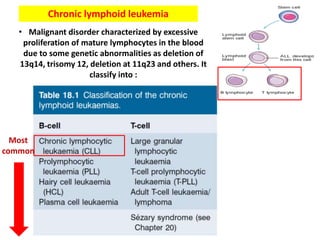
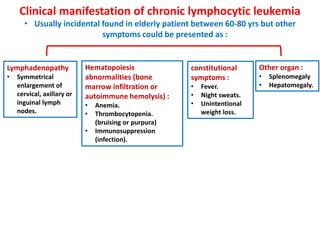
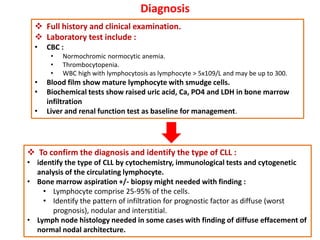
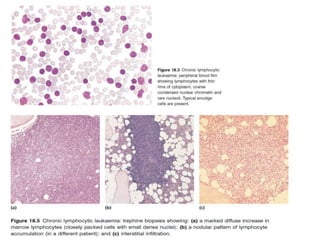
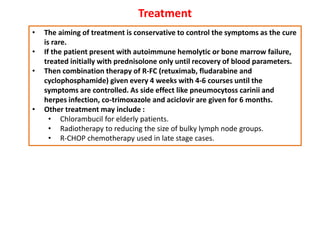
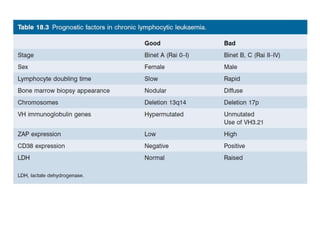
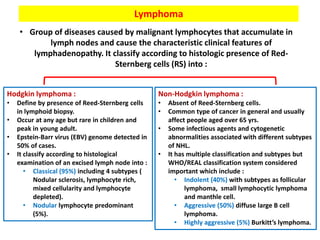
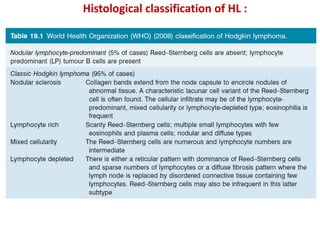
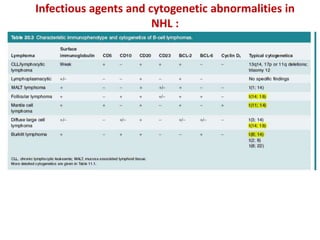
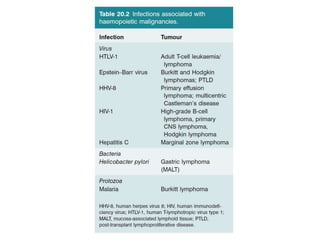
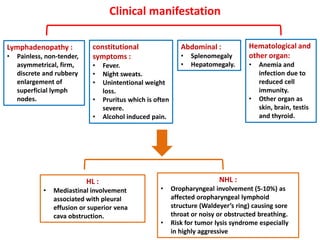
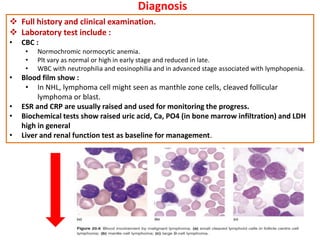
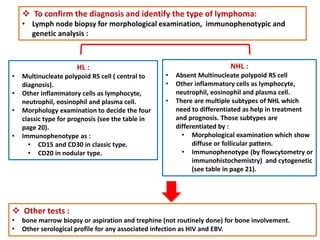
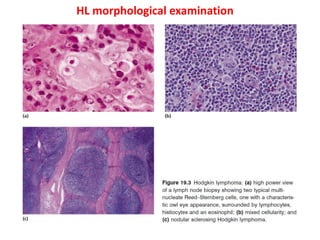
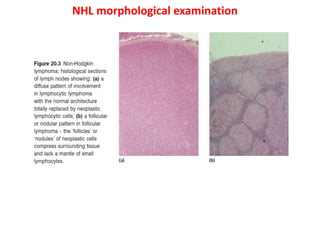
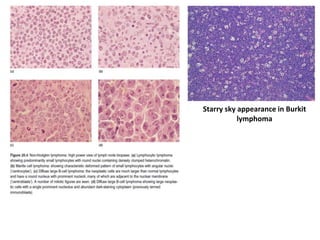
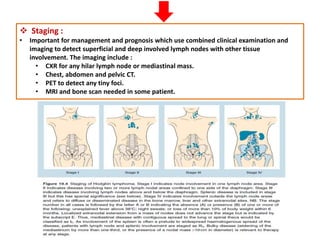
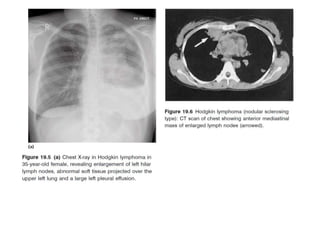
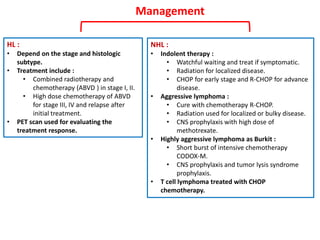
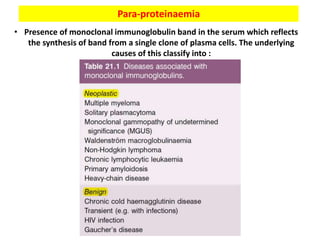
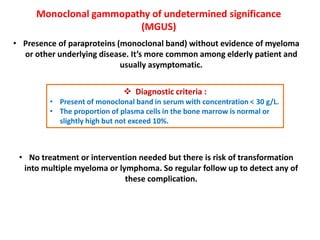
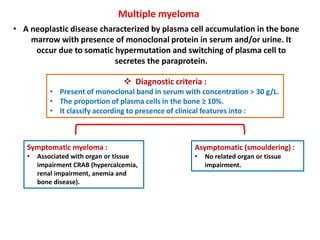
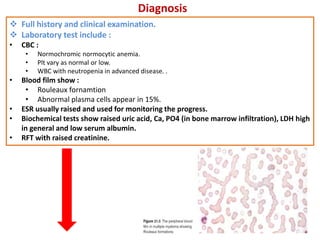
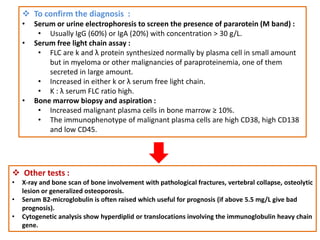
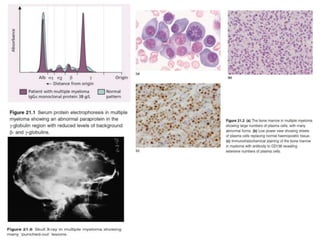
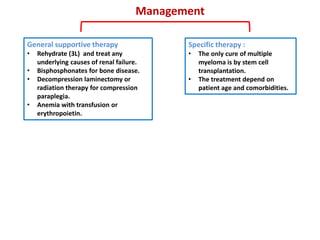
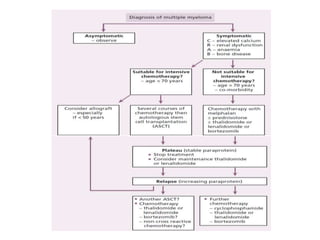
This document discusses lymphoid disorders including lymphoid malignancies such as acute lymphoblastic leukemia (ALL), chronic lymphocytic leukemia (CLL), lymphoma, and multiple myeloma. It provides details on the classification, clinical manifestations, diagnosis, and management of each condition. ALL is characterized by excessive lymphoblast proliferation and can be T-cell or B-cell subtype. CLL is a malignant disorder of mature lymphocytes in blood. Lymphoma is caused by malignant lymphocytes accumulating in lymph nodes. Multiple myeloma is a plasma cell neoplasm characterized by monoclonal protein in serum/urine and bone lesions.