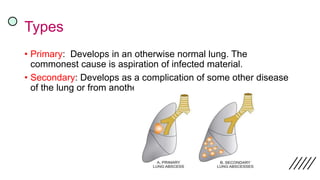
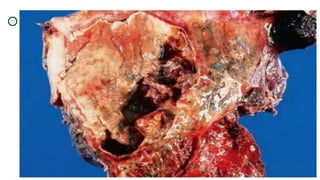
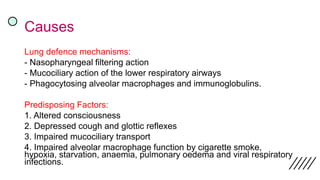
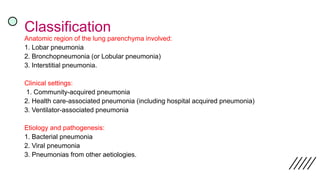
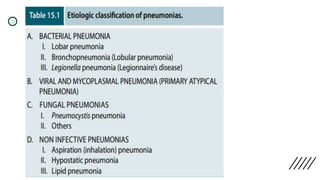
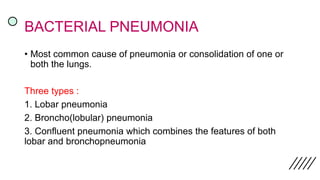
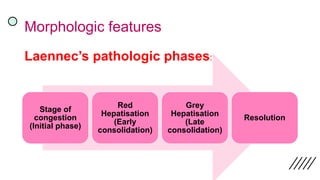
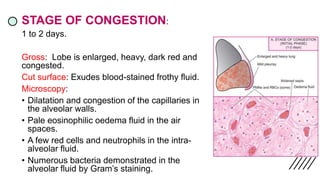
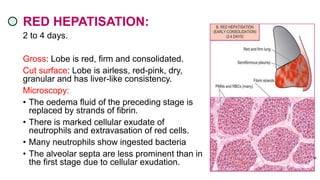
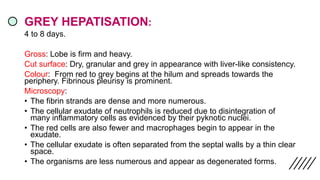
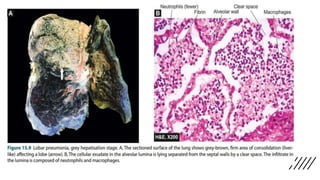
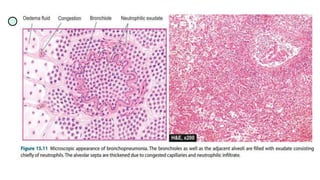
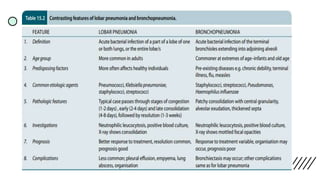
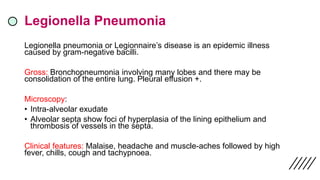
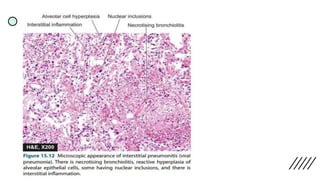
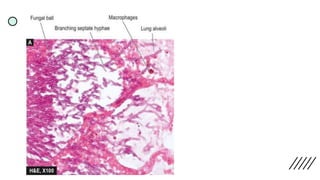
The document discusses lung abscesses and pneumonia, detailing their definitions, causes, clinical features, morphology, complications, and treatment methods. Lung abscesses may arise from several infections and lead to symptoms such as cough and hemoptysis, while pneumonia represents an acute lung inflammation with various causative pathogens, manifesting in different clinical settings. The text also covers the different types of pneumonia, their paths of development, and associated complications, emphasizing the need for antibiotic treatment and possible surgical interventions.