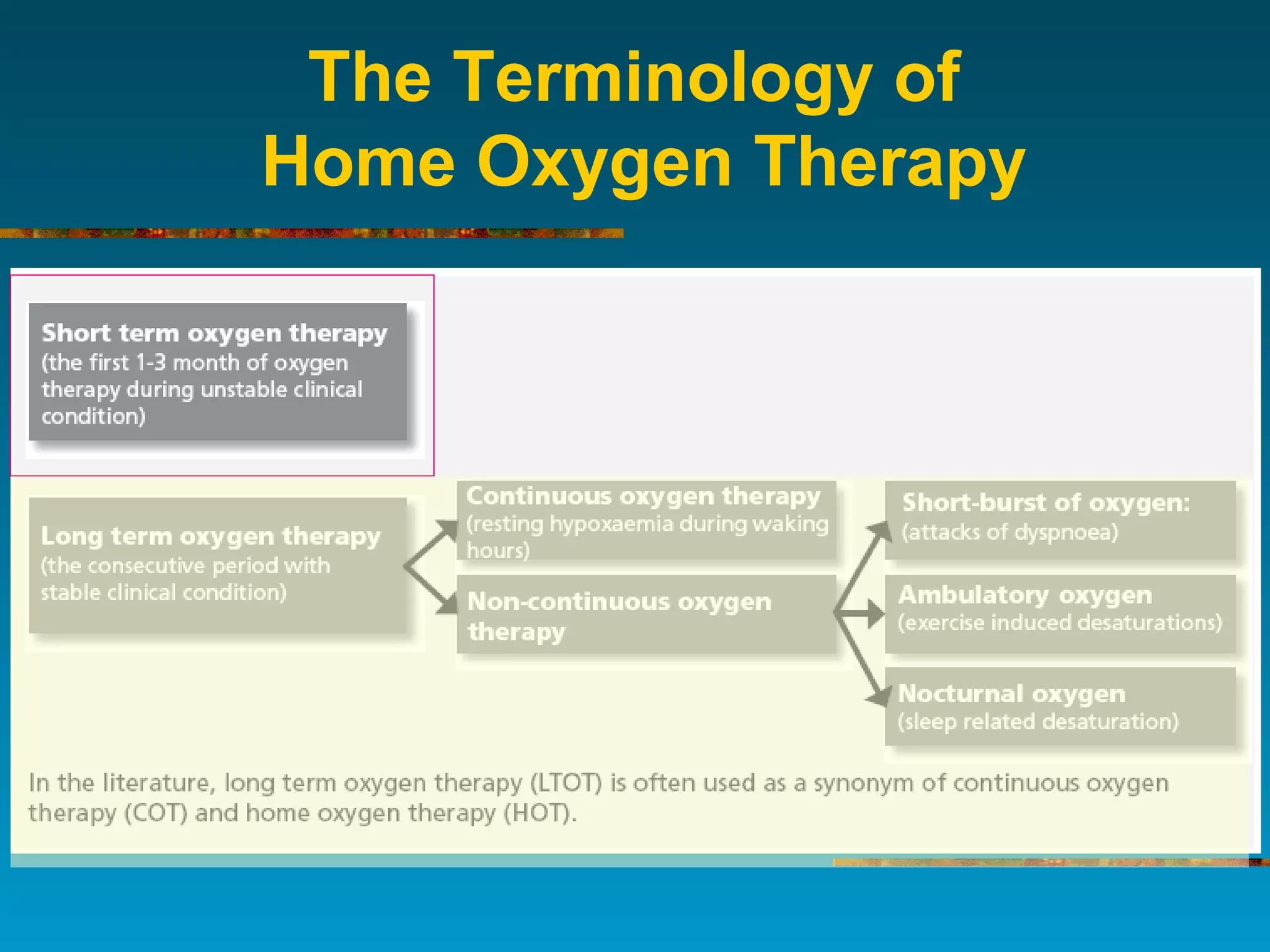
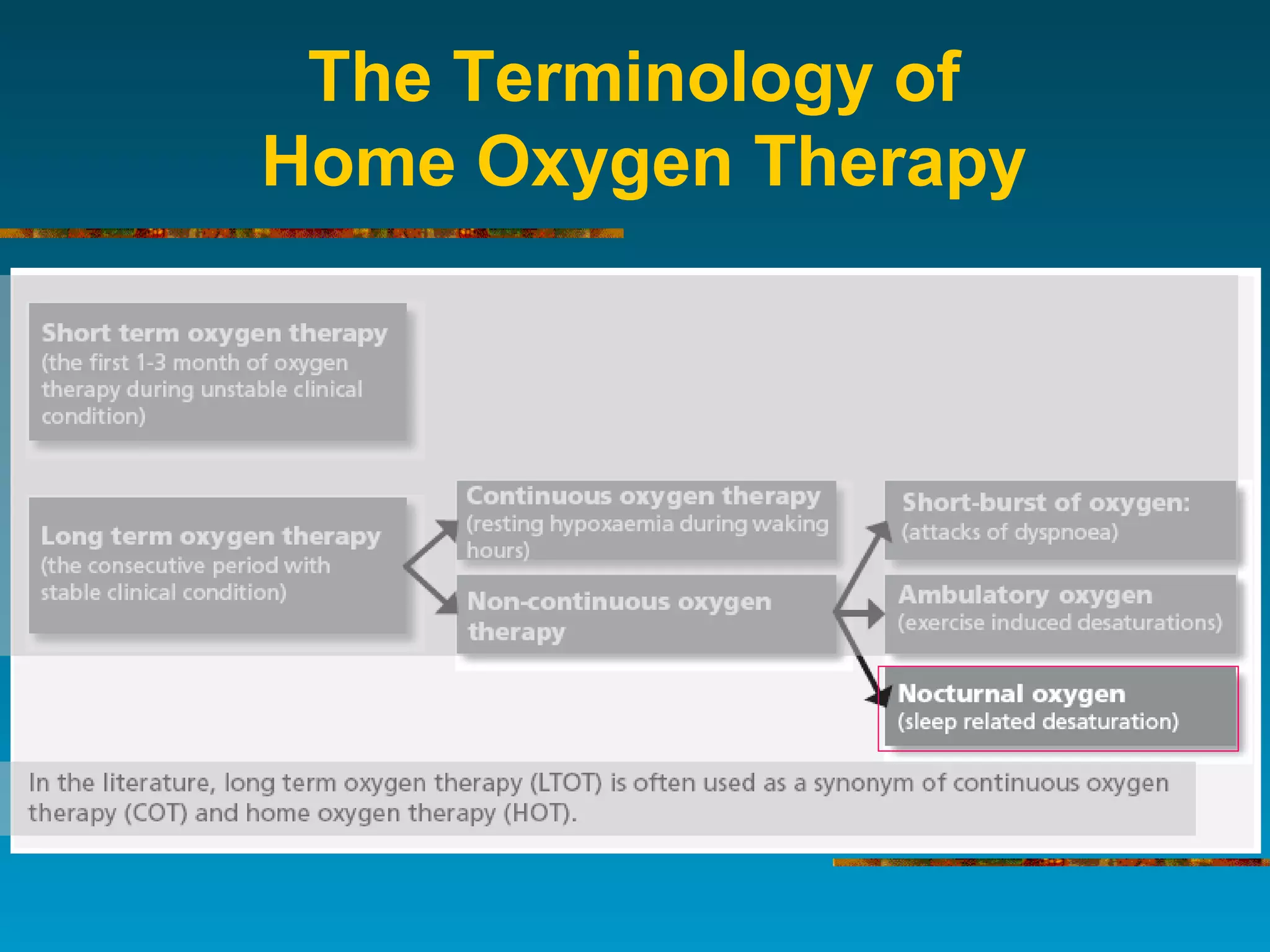
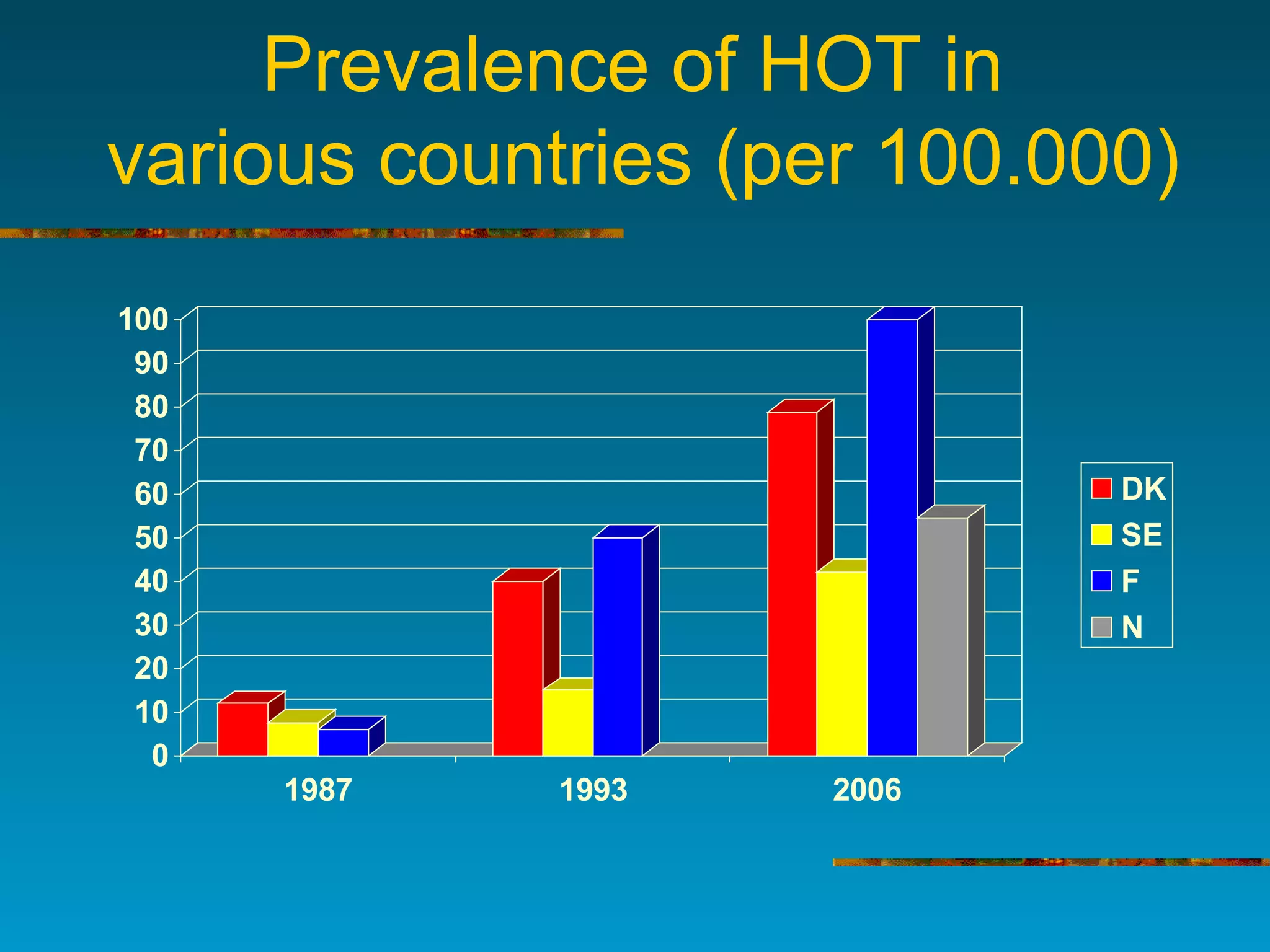
1) Home oxygen therapy (HOT) improves survival in patients with hypoxemia, though adherence to guidelines and follow-up is only about 50% in many countries.
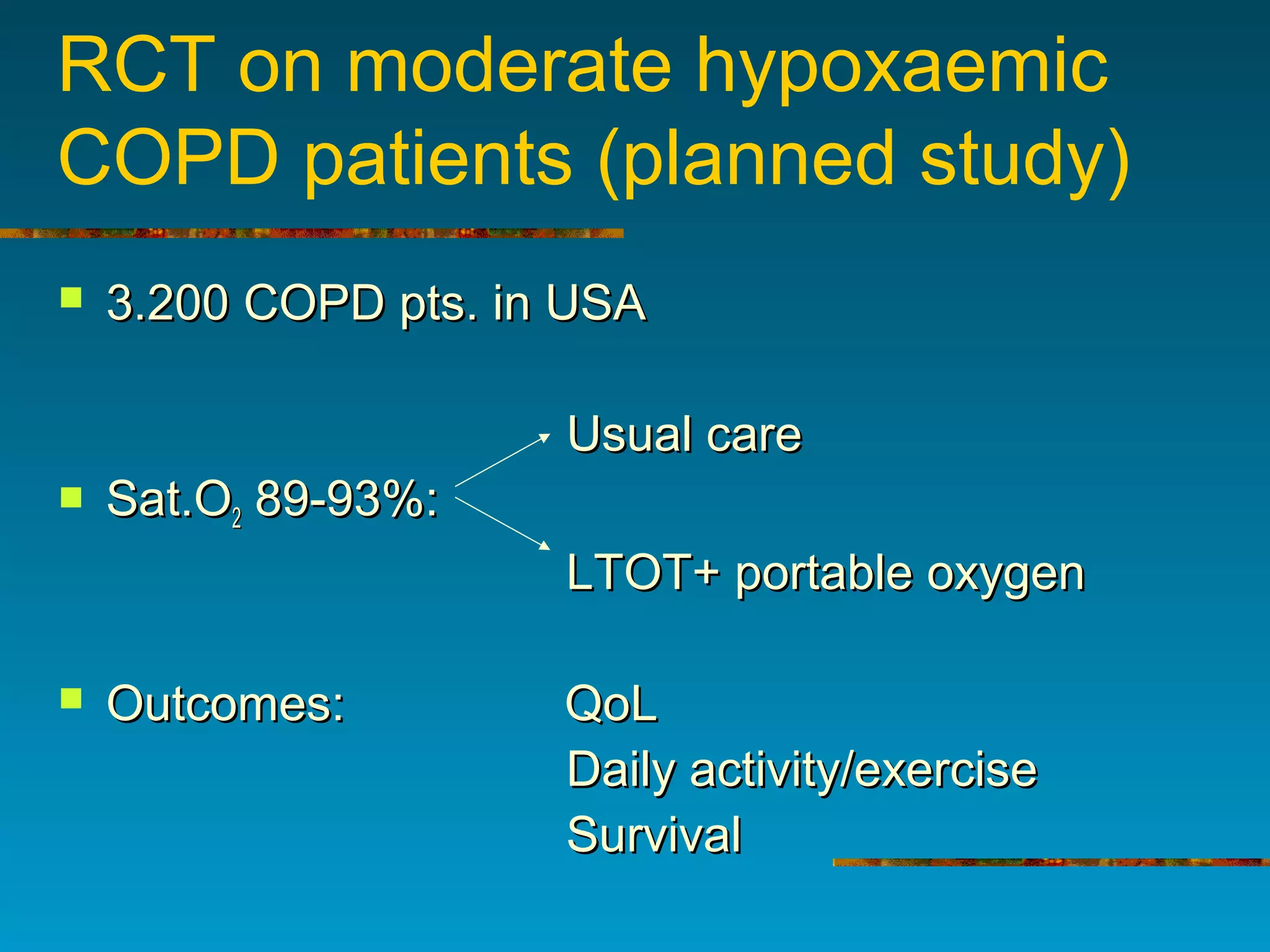
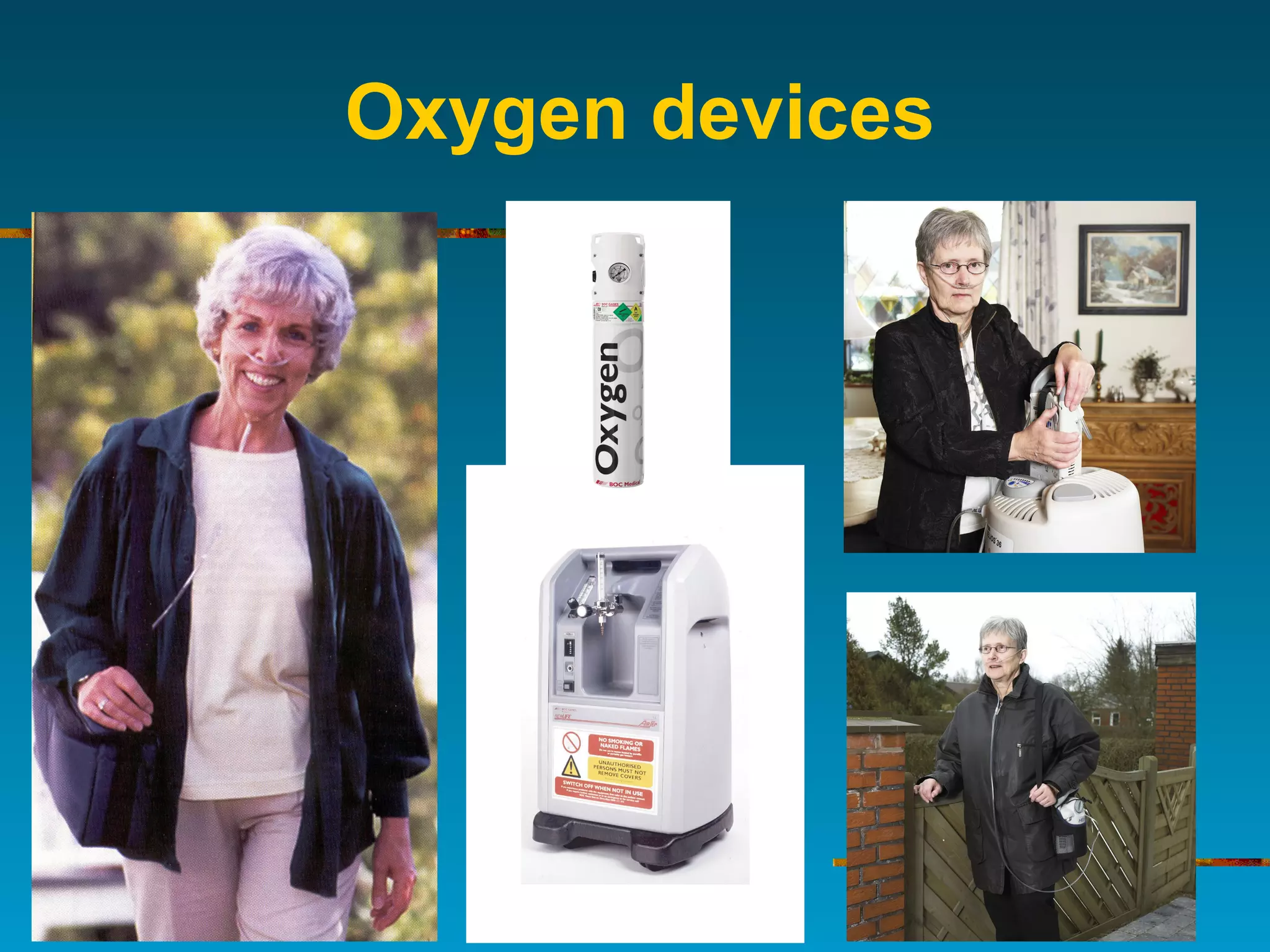
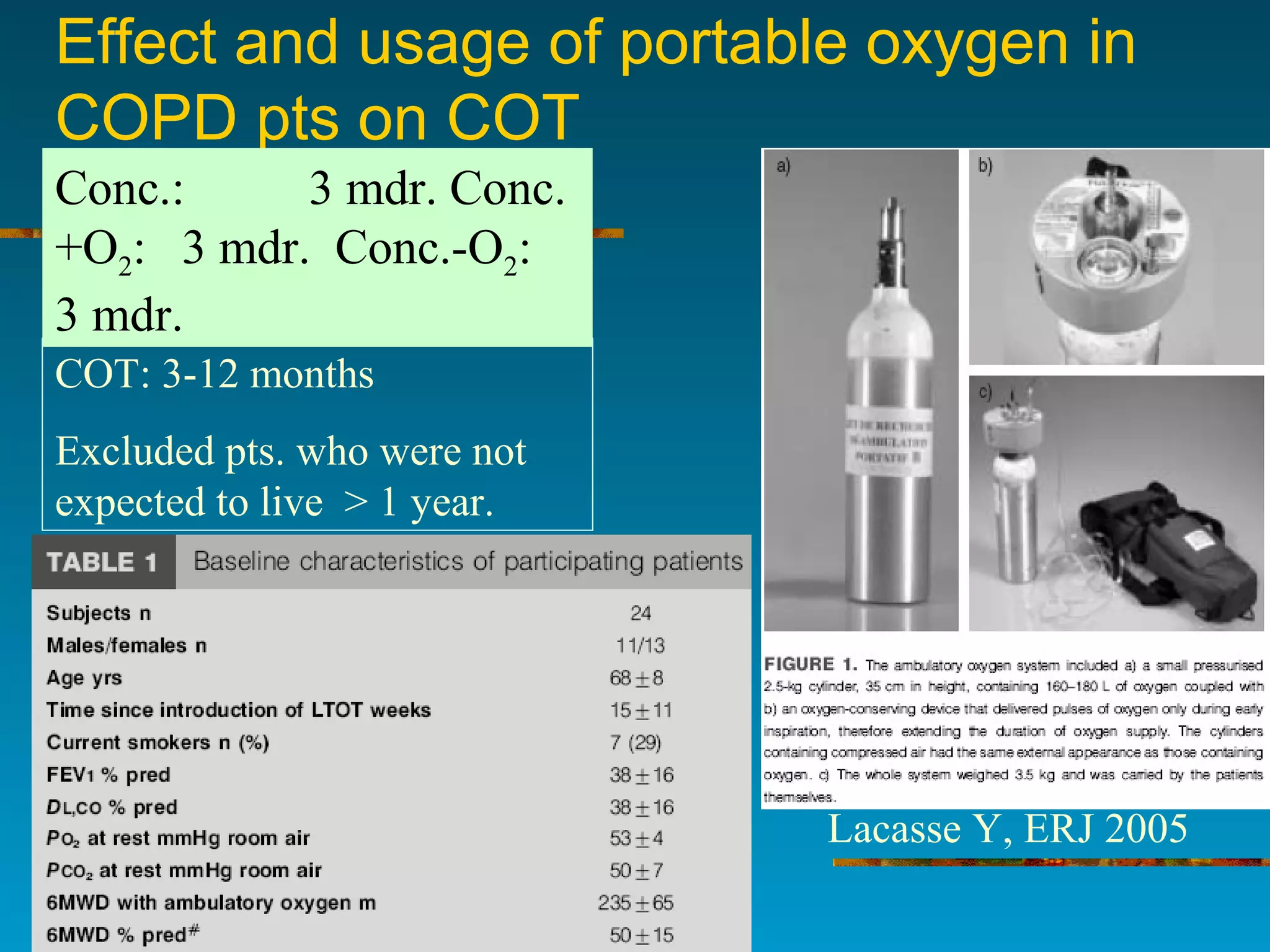
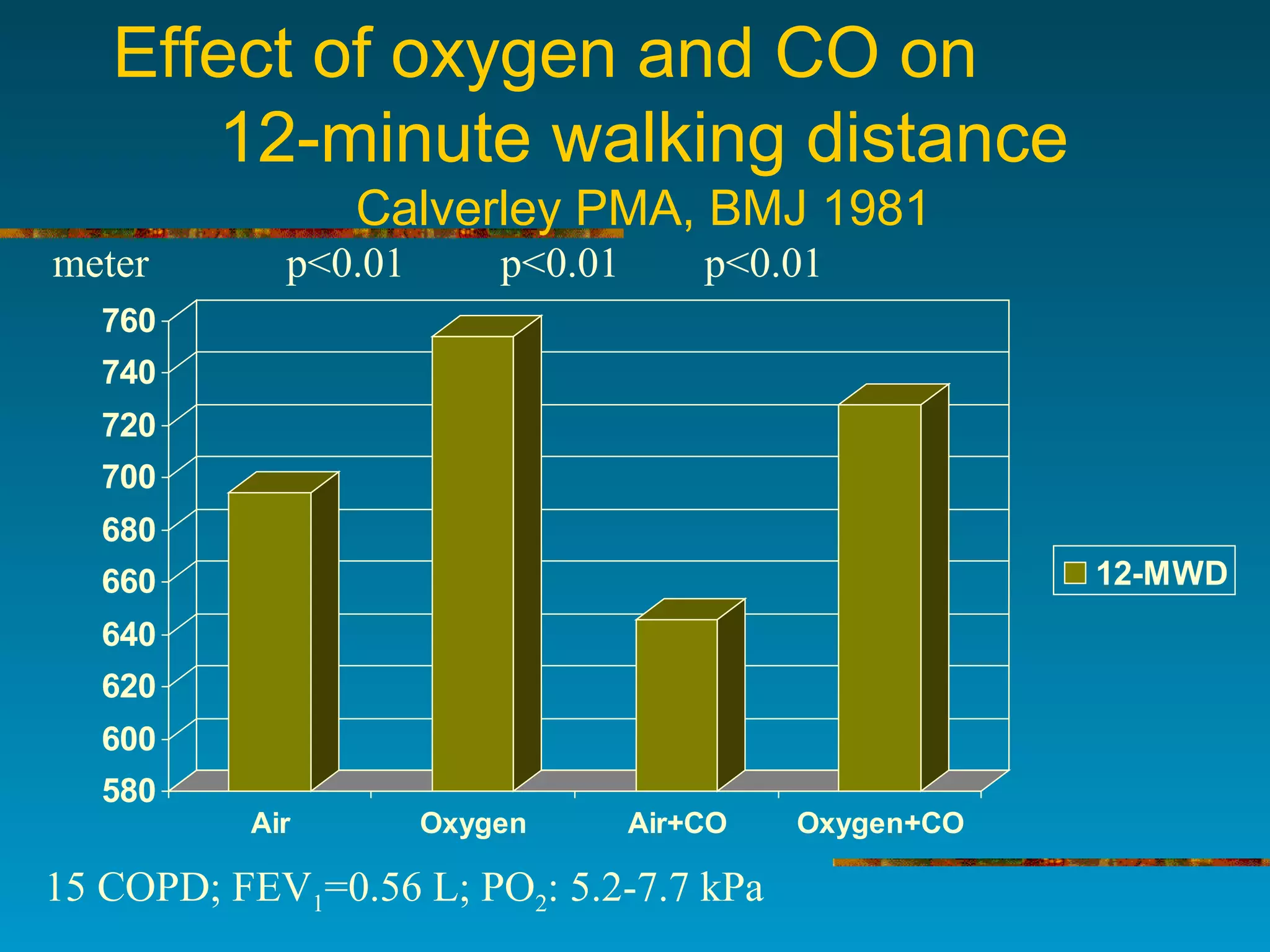
2) Continuous oxygen therapy (COT) given for over 15 hours daily increases survival by 2-4 years in COPD patients with low oxygen levels. Portable oxygen allows more activity but devices are still heavy.
3) International guidelines recommend COT for patients with oxygen levels below 7.3 kPa, but adherence varies, from 35-81% of eligible patients receiving treatment across different countries. Follow-up after starting COT is also inconsistent.