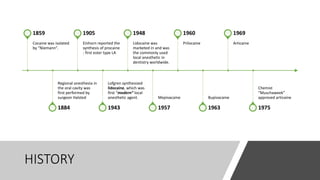
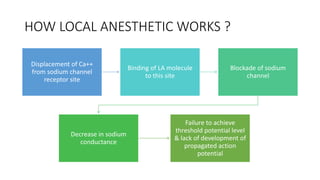
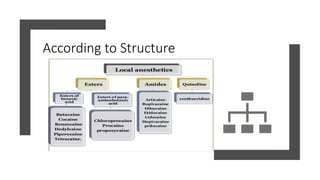
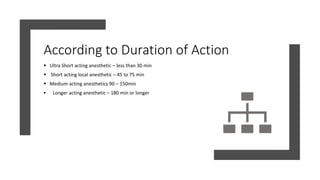
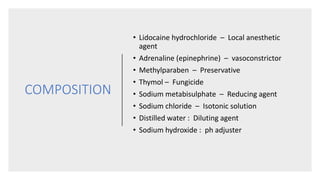
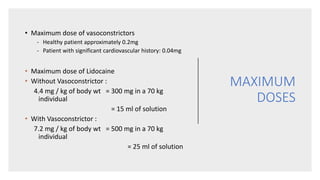
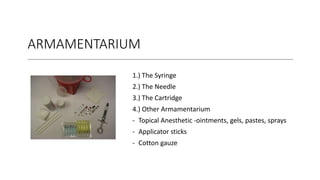
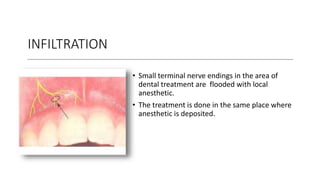
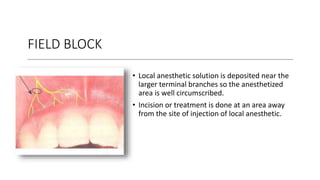
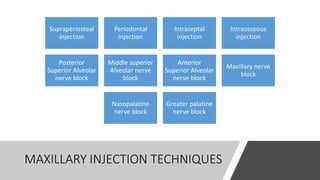
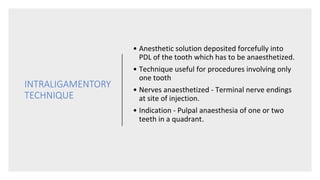
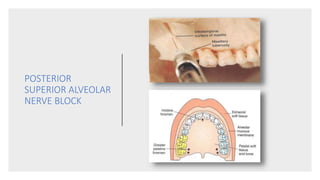
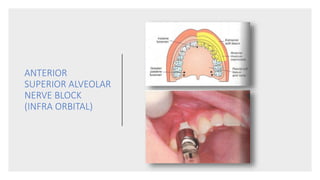
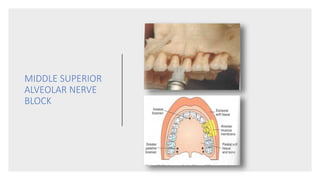
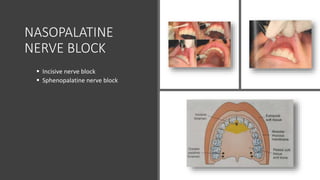
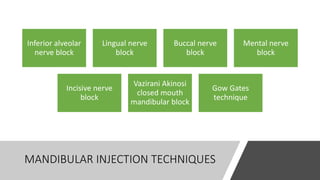
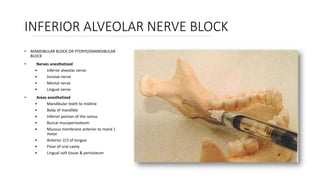
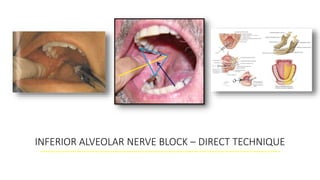
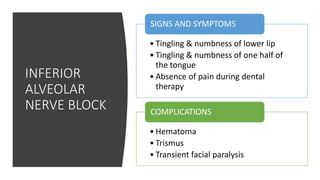
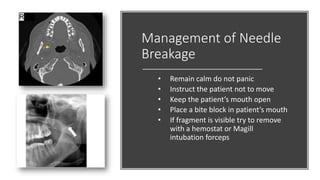
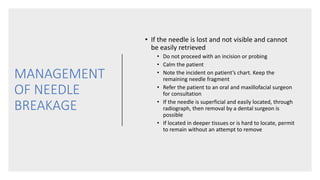
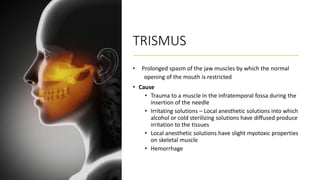
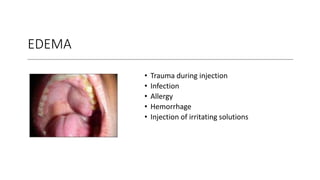
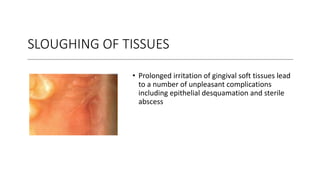
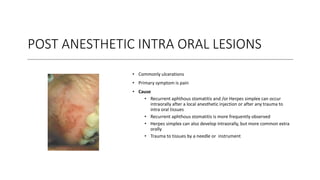
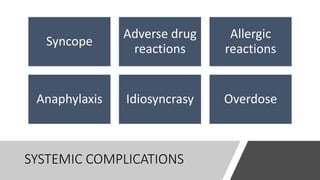
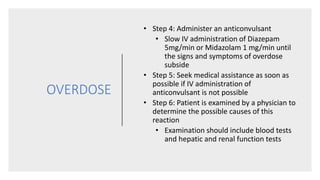
This document provides an overview of local anesthesia. It begins with definitions of local anesthesia and discusses its history from the isolation of cocaine in 1859 to the development of modern local anesthetics like lidocaine. It describes the ideal properties, theories of action, classification, composition, maximum doses, armamentarium, techniques for maxillary and mandibular injections, and potential complications. The key information is that local anesthesia temporarily interrupts nerve conduction to produce loss of sensation in a circumscribed area, allowing for painless dental procedures.