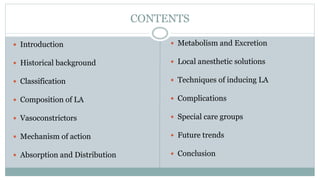
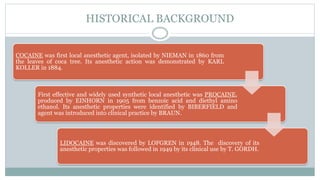
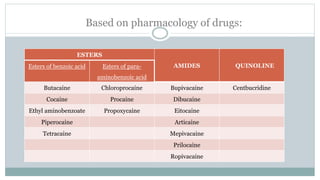
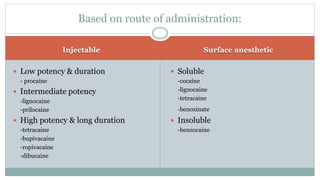
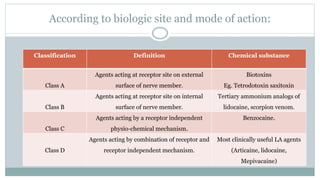
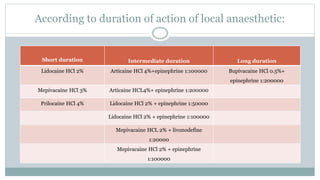
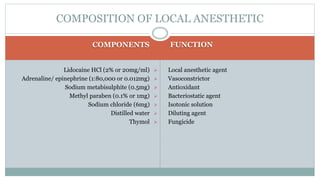
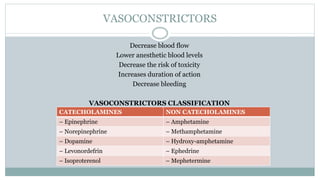
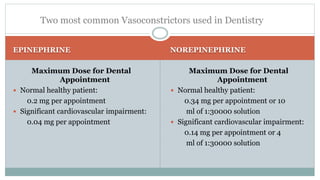
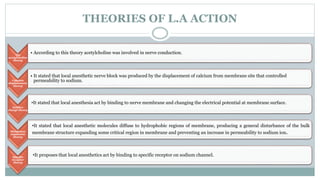
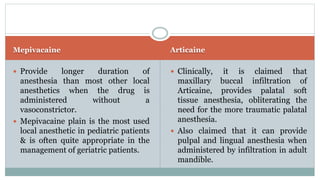
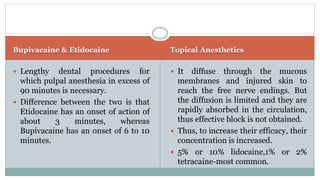
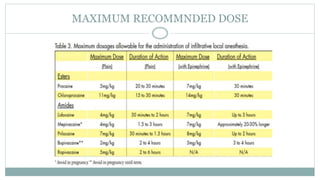
This document provides an overview of local anesthesia. It begins with definitions and an introduction. It then covers the historical background, classifications, components, mechanisms of action, techniques, and complications of local anesthesia. The classifications section divides local anesthetics based on their pharmacology, route of administration, biologic site and mode of action, and duration of action. Key local anesthetic agents like lidocaine, mepivacaine, articaine, bupivacaine, and topical anesthetics are also summarized. Maximum recommended doses and specific nerve block techniques for the maxillary nerve are outlined. In conclusion, the document reviews local anesthesia in detail.

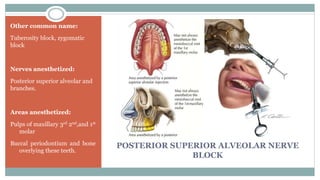
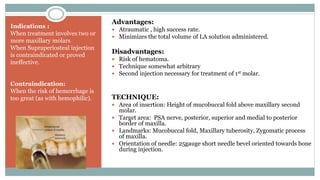
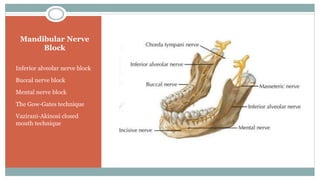
![TECHNIQUES OF INJECTING LOCAL ANESTHESIA
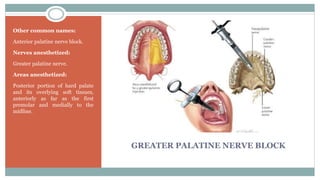
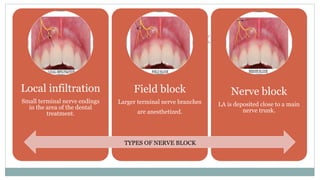
Supraperiosteal [infiltration], recommended for limited treatment protocols.
Periodontal ligament [ PDL, intraligamentary] injection, recommended as adjunct to
other techniques.
Intraseptal injection, recommended primarily for periodontal surgical techniques.
Intracrestal injection, recommended for single teeth [primarily mandibular molars].
Intraosseous injection, recommended for single teeth [primarily mandibular molars].](https://image.slidesharecdn.com/localanesthesia-240327081209-16a3866b/85/local-anesthesia-Uses-Types-Side-effects-and-Safety-23-320.jpg)
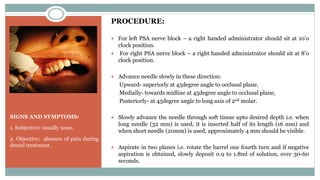
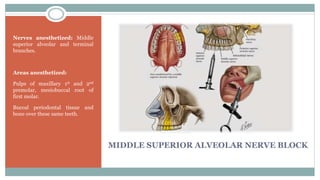
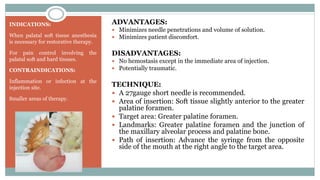
![Maxillary Nerve
Block
Posterior superior alveolar
[PSA] nerve block
Middle superior alveolar
[MSA] nerve block
Anterior superior alveolar
[ASA, infraorbital] nerve
block
Greater palatine nerve block
Nasopalatine nerve block](https://image.slidesharecdn.com/localanesthesia-240327081209-16a3866b/85/local-anesthesia-Uses-Types-Side-effects-and-Safety-24-320.jpg)