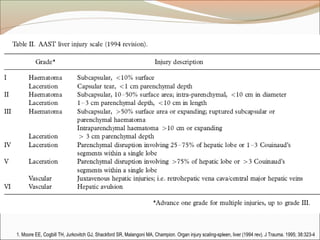
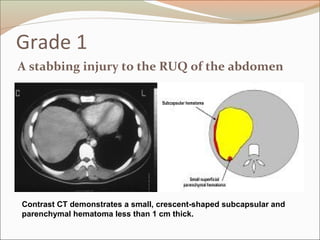
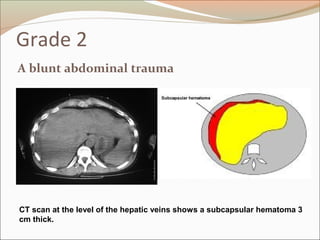
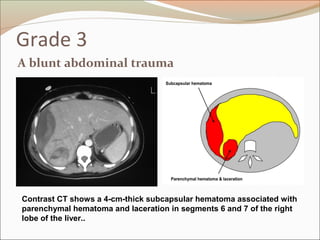
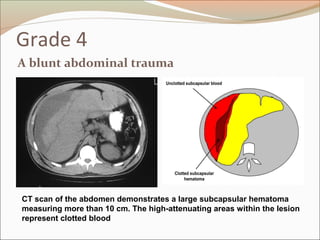
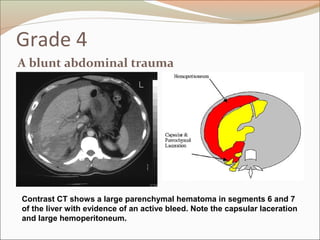
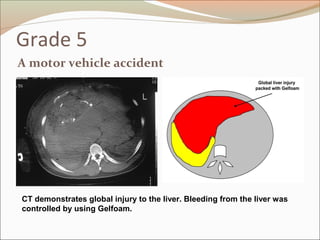
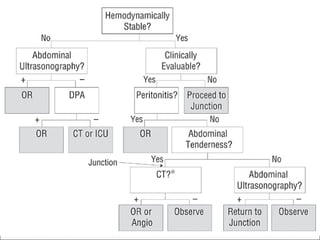
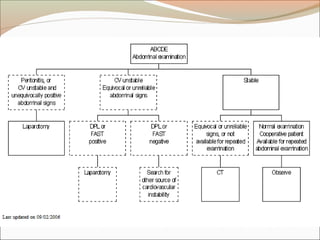
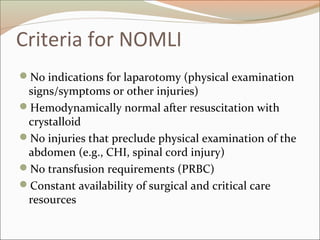
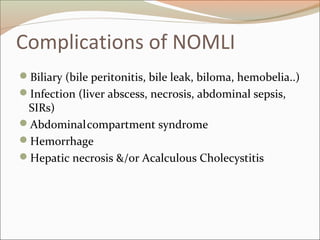
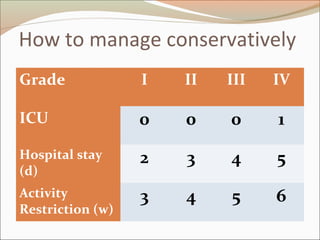
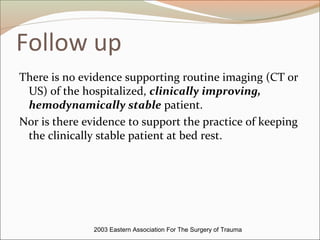
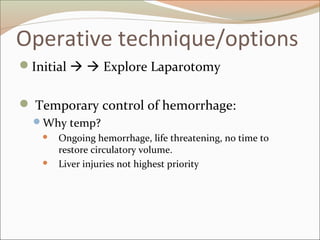
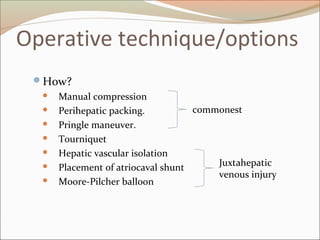
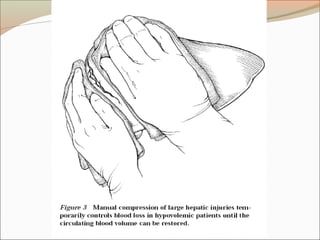
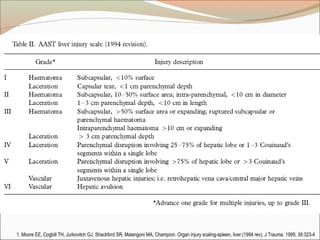
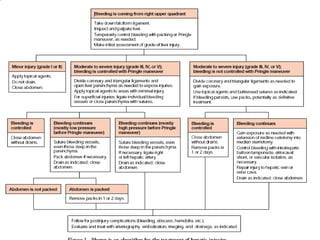
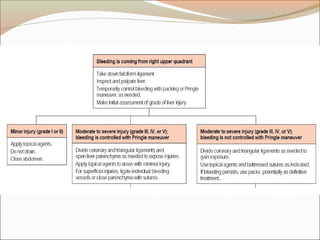
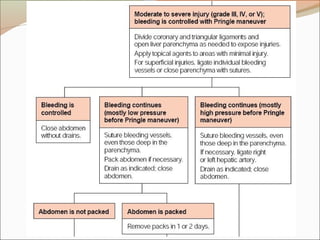
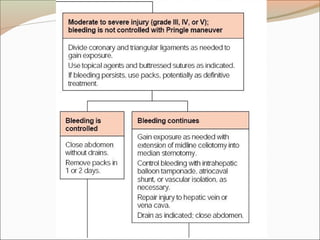
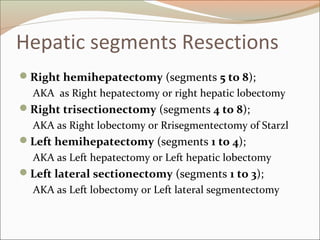
This document provides an overview of liver anatomy, physiology, and management of liver trauma. It describes the surface anatomy, blood supply, ligaments, segments, and imaging appearance of the liver. Factors making the liver prone to injury are discussed. Grades of liver injuries based on the Moore scale are outlined with examples. Non-operative and operative management strategies are reviewed, including criteria for each approach and techniques for temporary and definitive control of hemorrhage. Complications of non-operative management and indications for failure are also summarized.
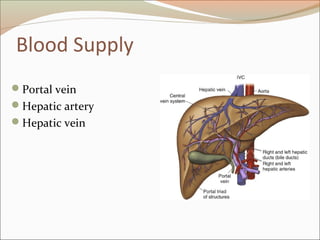
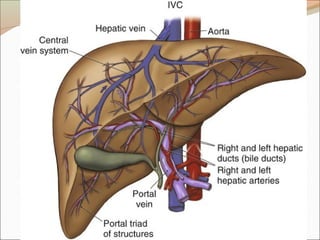
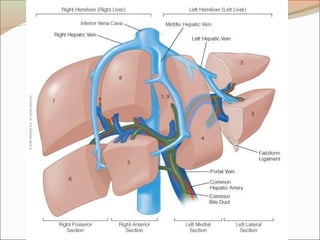
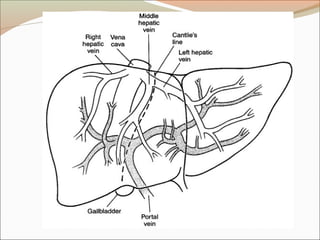
![Blood supply – Hepatic vein
Rt hepatic vein Drain seg 5,6,7,8 vena cava.
Middle hepatic vein Drain seg 4,5,8
Lt hepatic vein Drain seg 2,3
[ seg 1 drain by short hepatic vena cava]](https://image.slidesharecdn.com/appliedliveranatomy-091219152729-phpapp01-140406135920-phpapp02/85/Appliedliveranatomy-091219152729-phpapp01-23-320.jpg)