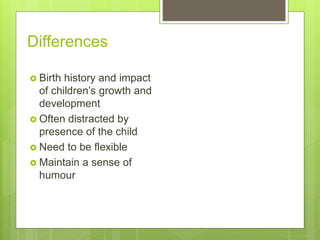
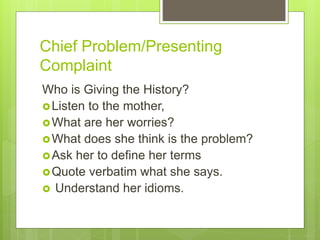
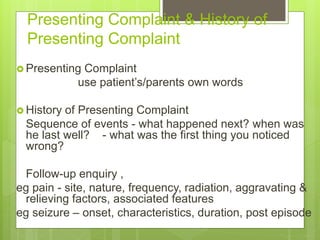
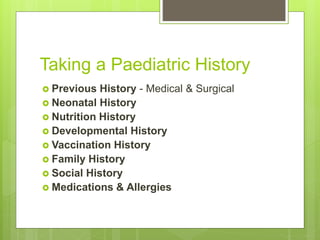
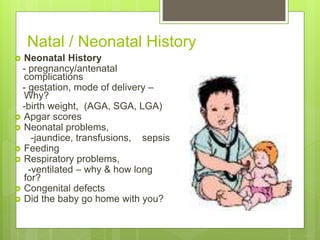
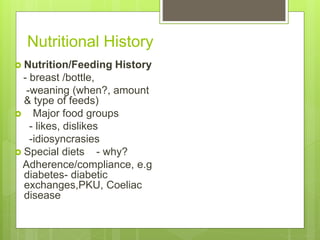
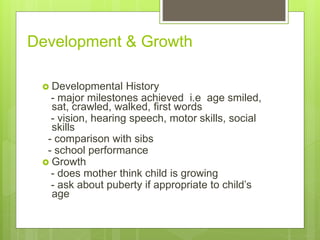
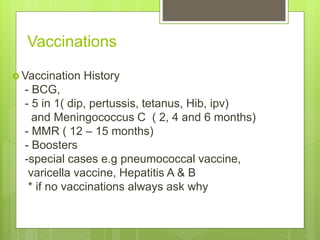
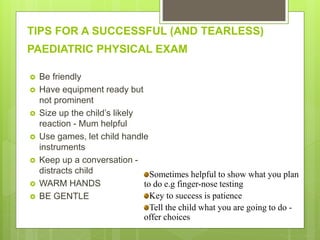
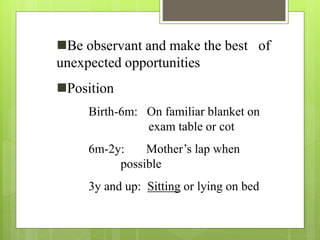
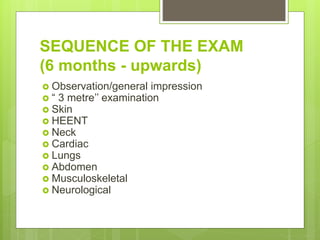
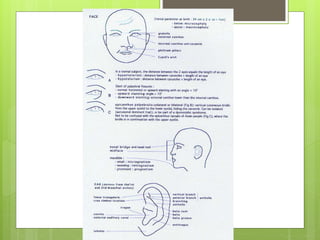
The document provides guidance on taking a pediatric history, including focusing the history on the chief complaint, birth and medical history, developmental milestones, vaccinations, family history, and social factors. It also outlines the approach to performing a physical examination of children, with tips on techniques for different age groups and examining individual body systems in a sensitive manner. The goal is to obtain relevant information to identify health issues while maintaining the comfort, safety and dignity of pediatric patients.