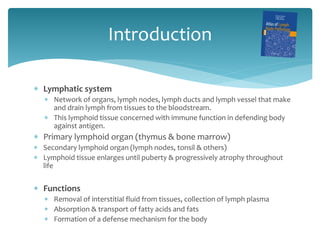
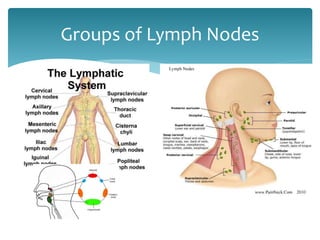
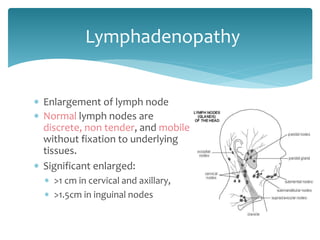
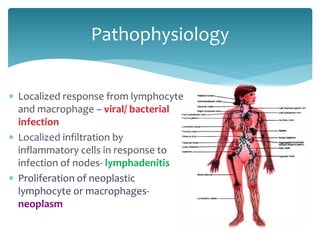
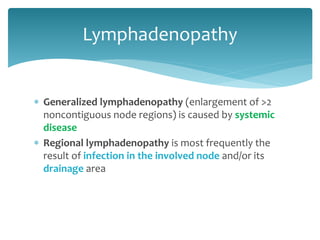
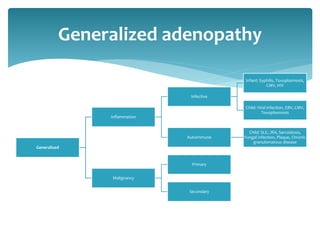
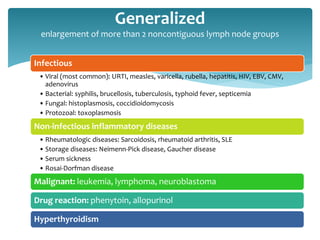
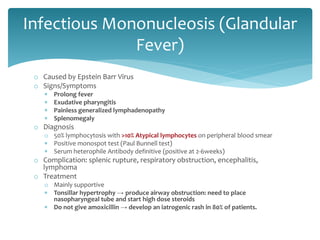
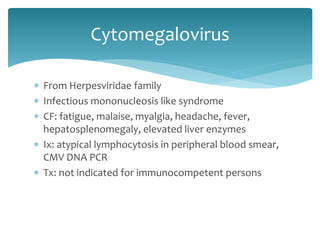
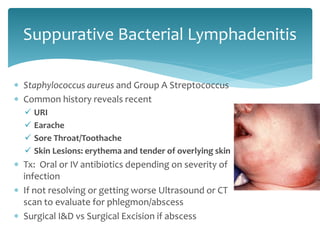
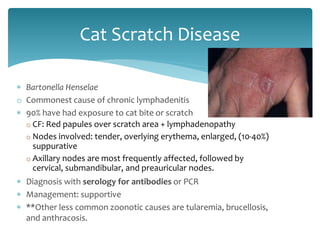
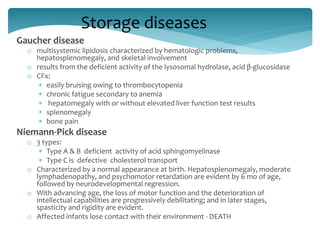
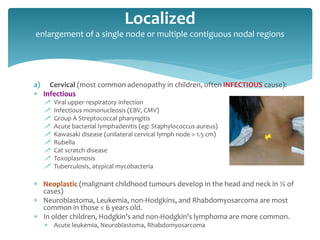
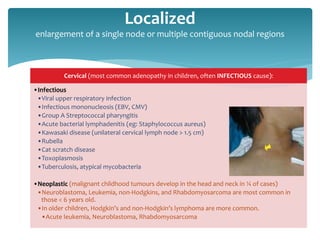
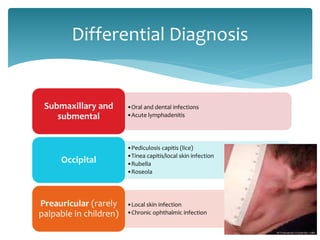
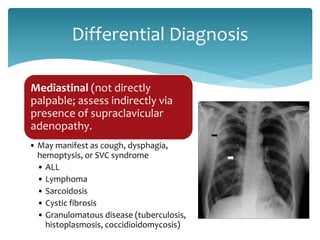
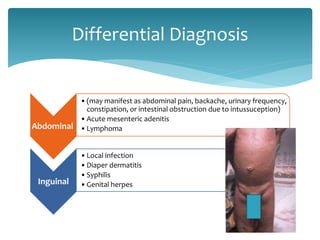
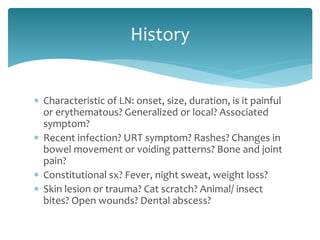
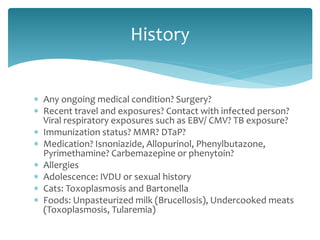
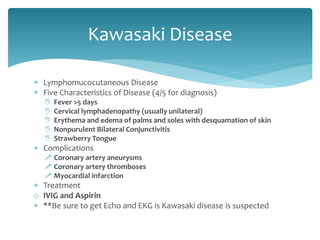
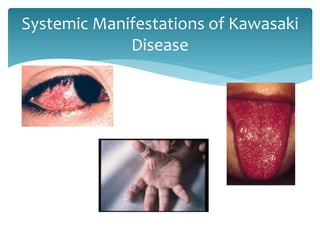
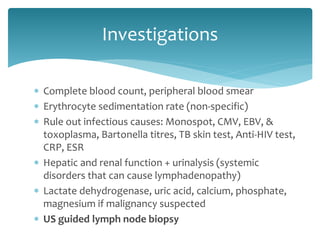
This document discusses the approach to a child presenting with lymphadenopathy. It begins with an introduction to lymph node anatomy and pathophysiology. It then discusses the differential diagnosis and key features of generalized versus regional lymphadenopathy. Specific infectious, inflammatory and malignant conditions that can cause lymphadenopathy are outlined. The summary concludes with guidance on taking a thorough history to identify potential causes and guide appropriate investigations.