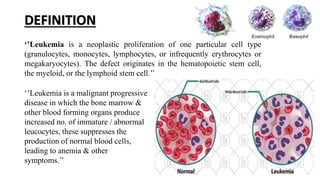
The document discusses leukemia, which is a cancer of the blood and bone marrow. It defines leukemia as an abnormal proliferation of white blood cells. It then classifies leukemias as either acute or chronic, depending on how quickly symptoms develop, and as either lymphocytic or myeloid, depending on the affected cell type. The four main types of leukemia are described as acute lymphocytic leukemia, chronic lymphocytic leukemia, acute myeloid leukemia, and chronic myeloid leukemia. Clinical manifestations and nursing management are also outlined.