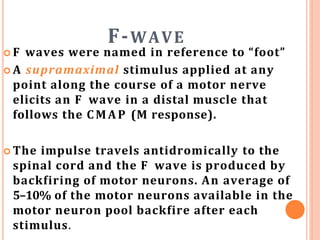
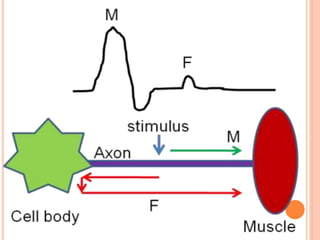
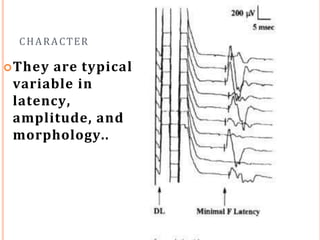
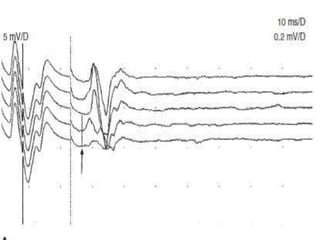
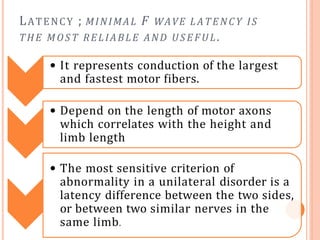
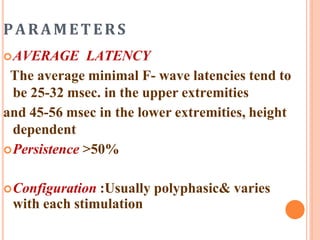
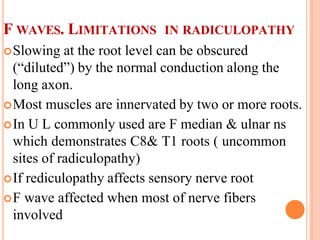
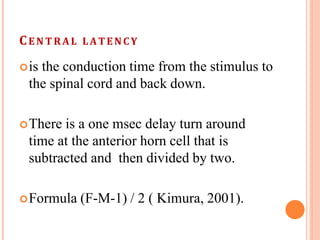
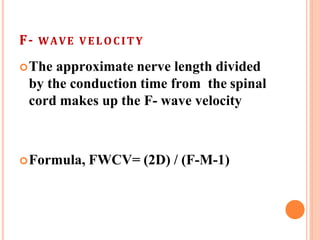
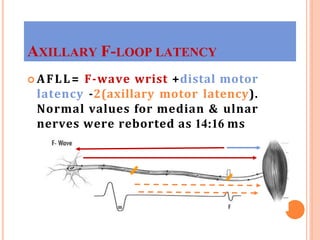
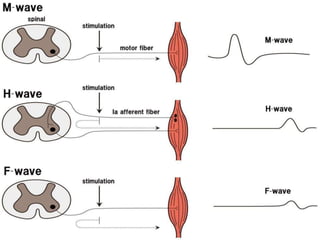
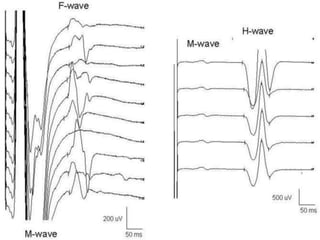
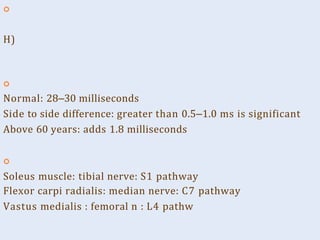
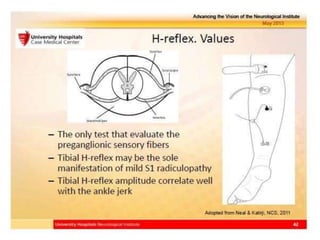
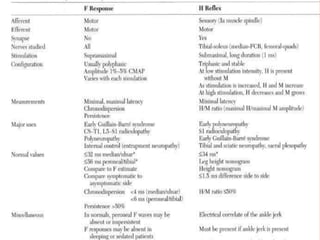
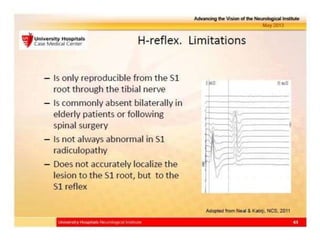
F waves are produced when a supramaximal stimulus is applied to a motor nerve, causing antidromic impulses that travel to the spinal cord. Some motor neurons then backfire, producing the F wave. F wave latencies provide information about motor nerve conduction velocity and can help detect neuropathies. The H-reflex is produced when a weak stimulus excites muscle spindle Ia afferents, causing antidromic impulses in the spinal cord that excite alpha motor neurons. F wave and H-reflex latencies are used to evaluate spinal and peripheral nerve conduction.