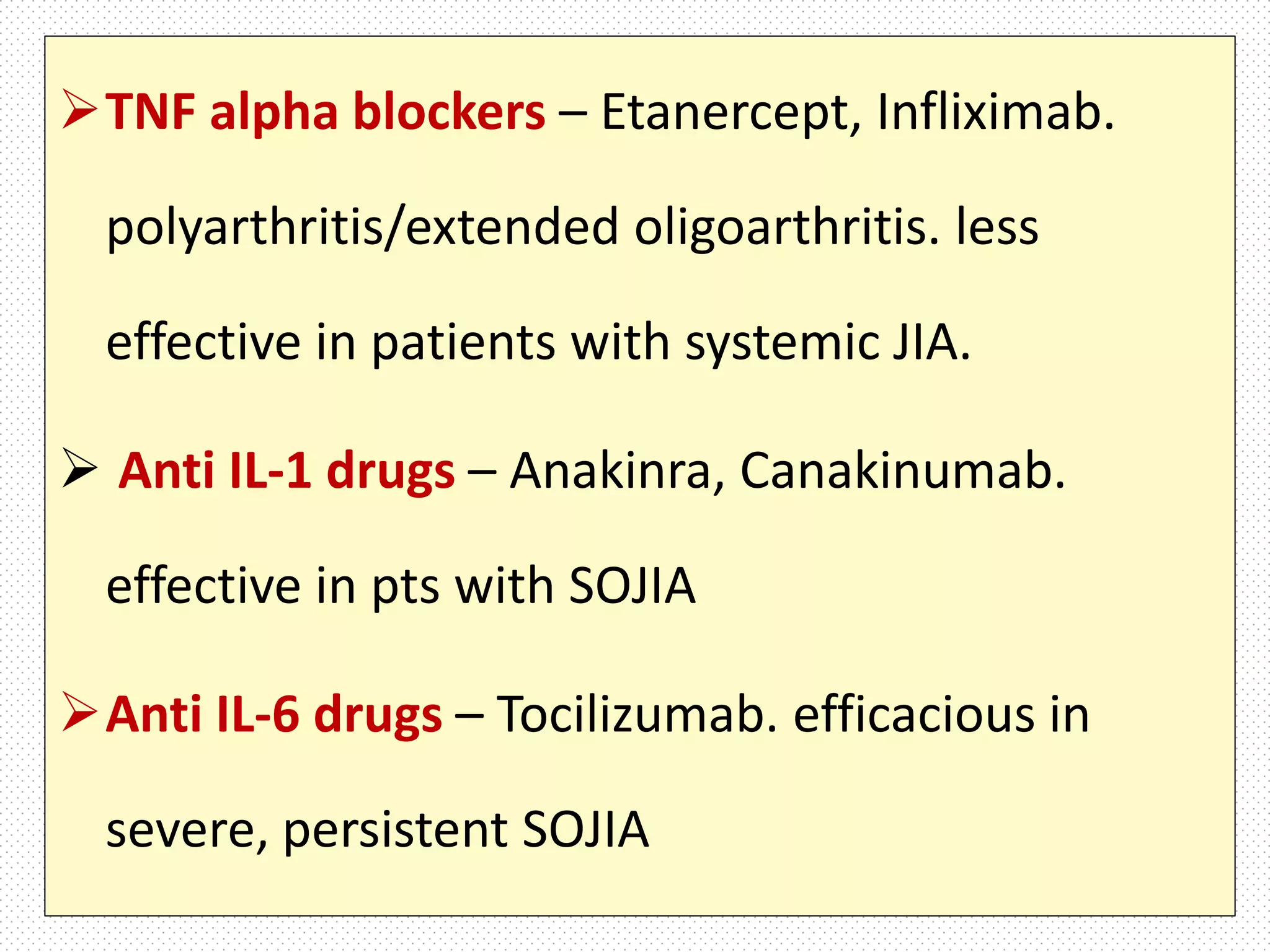
Juvenile Idiopathic Arthritis (JIA) is defined as arthritis of unknown cause that begins before age 16 and lasts over 6 weeks. It is classified based on symptoms into subtypes including systemic onset JIA, oligoarticular JIA, and polyarticular JIA. Treatment involves a stepwise approach starting with NSAIDs and intra-articular steroids and escalating to DMARDs and biologicals. Complications can include chronic anterior uveitis, osteoporosis, and potentially life-threatening macrophage activation syndrome.