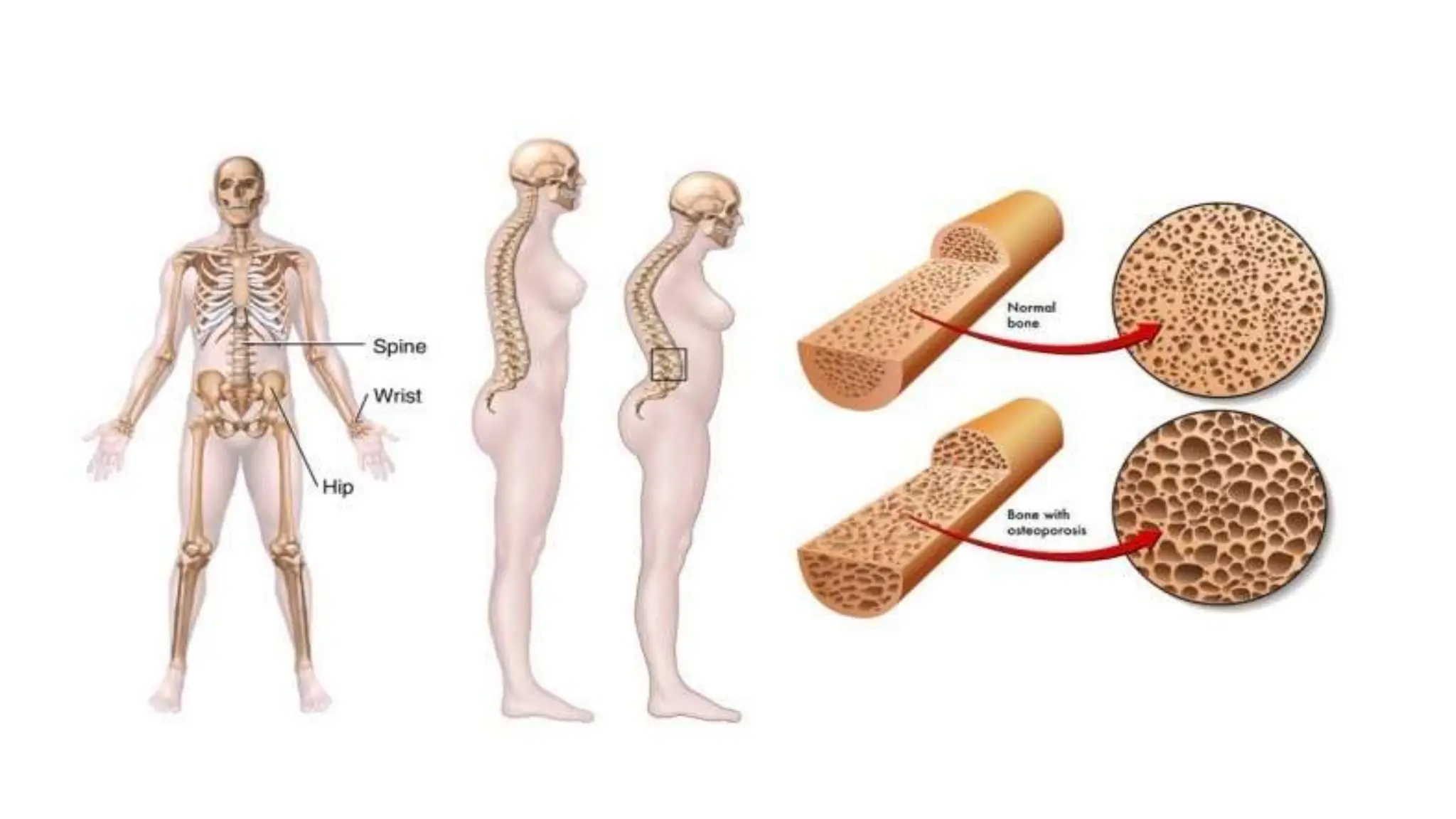
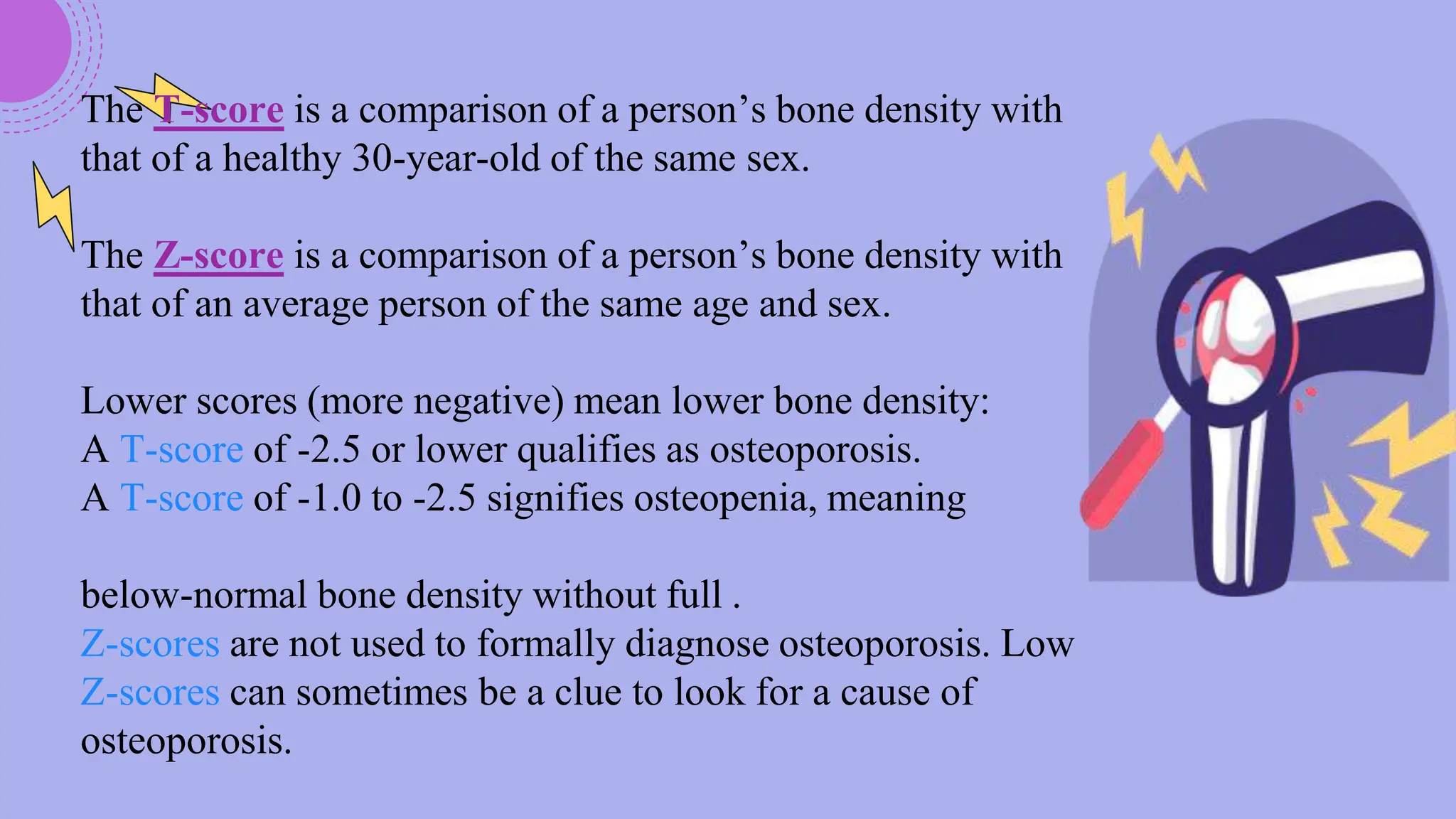
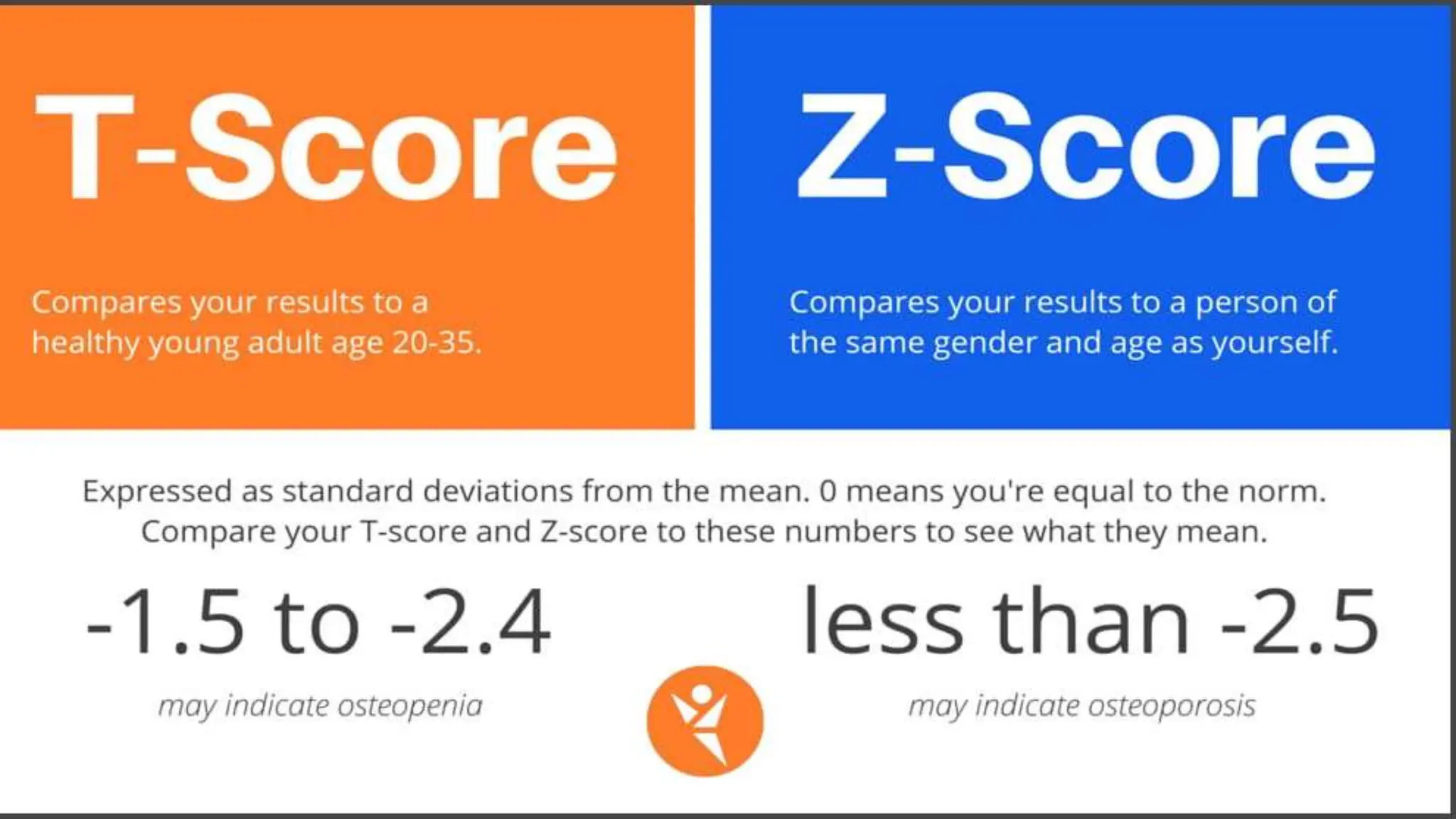
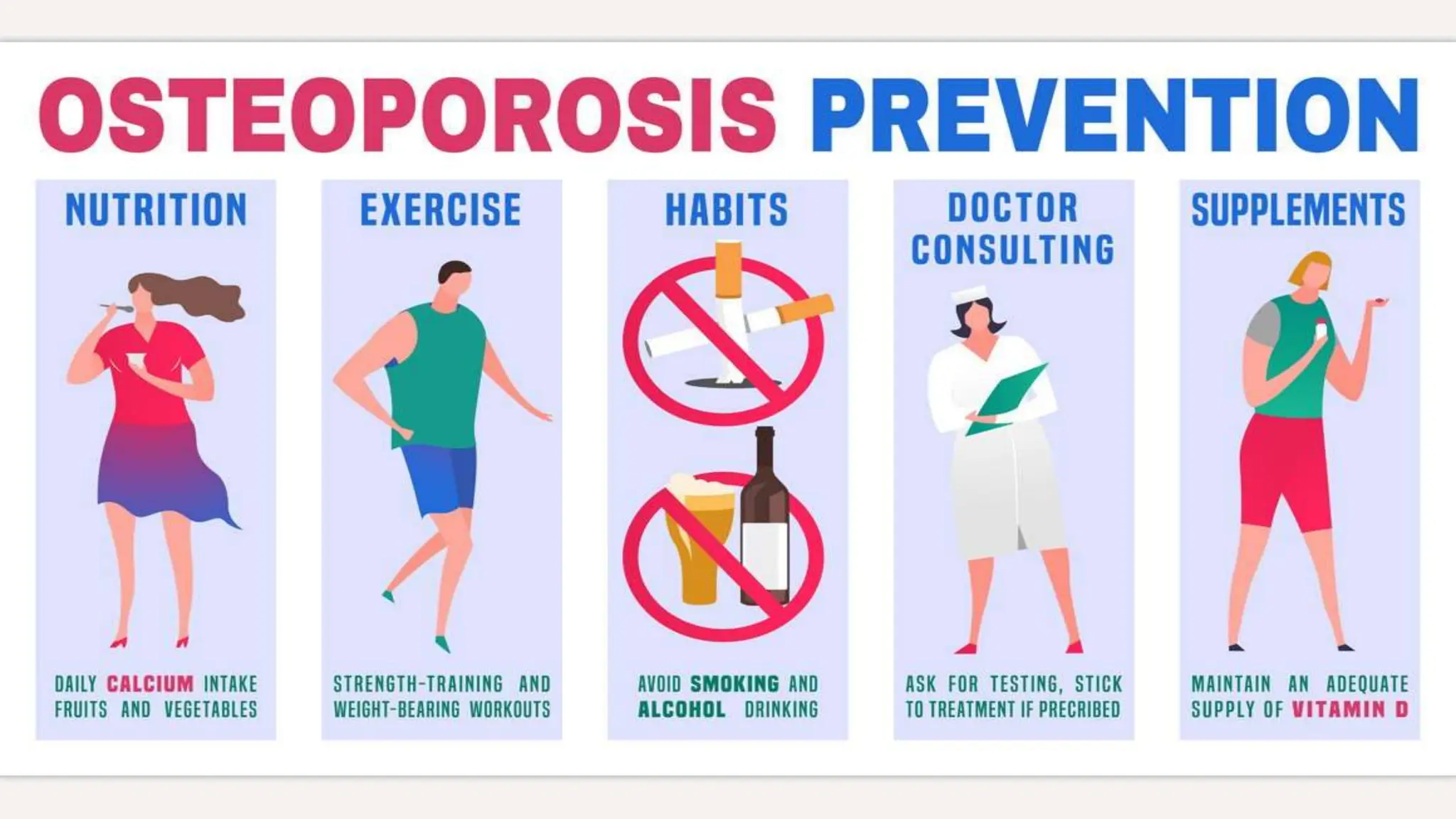
A 58-year-old postmenopausal woman presented with a left wrist fracture following a fall. Her medical history included asthma treated with corticosteroids, gastric ulcer, and a previous wrist fracture. Examination found a displaced, swollen wrist with no neurovascular compromise. X-ray revealed a Colles' fracture. Risk factors for osteoporosis from her history included advanced age, menopause, corticosteroid use, smoking, and lack of exercise. Further workup was needed to confirm the diagnosis and guide management, which may include bisphosphonates, parathyroid hormone, or calcium and vitamin D supplementation to prevent future fractures.