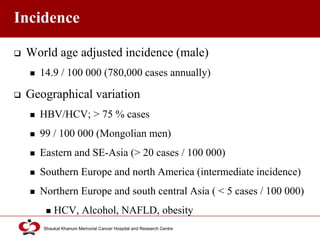
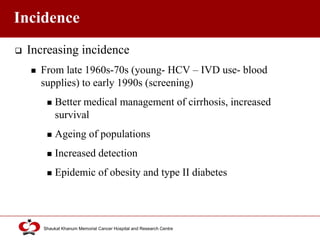
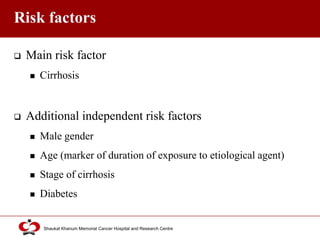
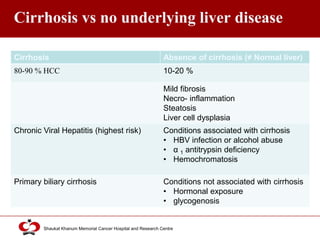
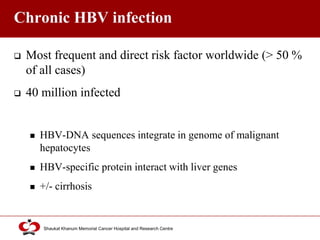
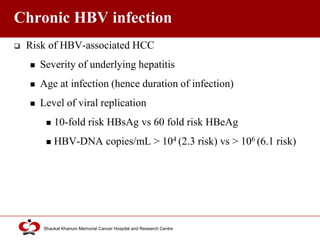
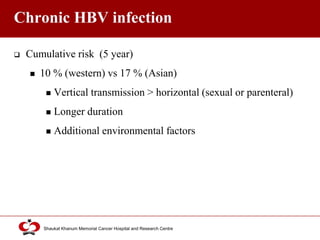
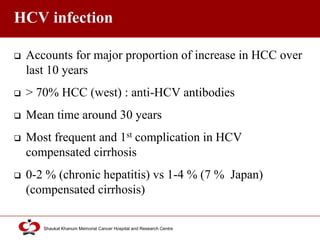
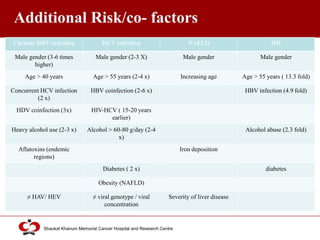
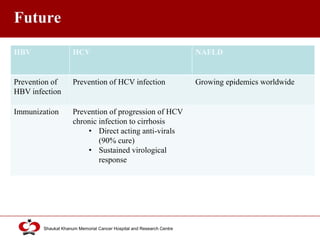
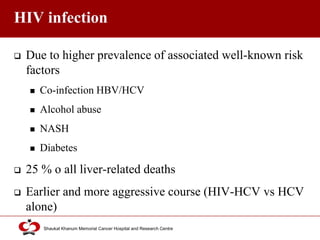
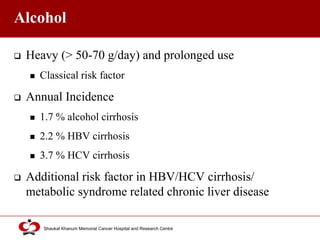
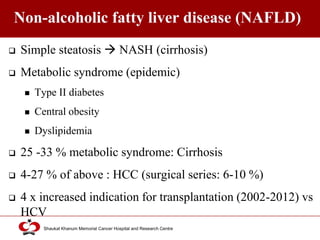
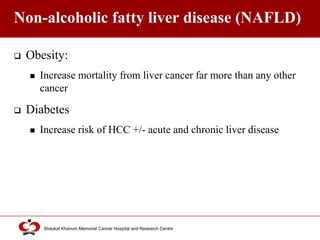
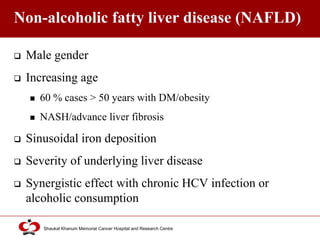
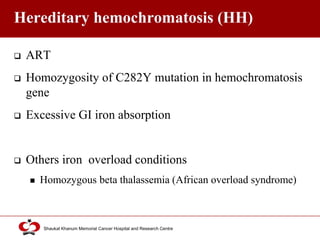
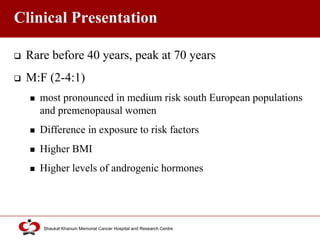
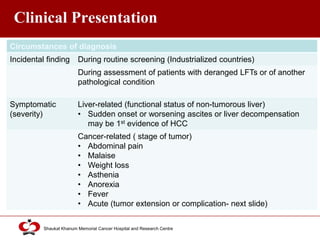
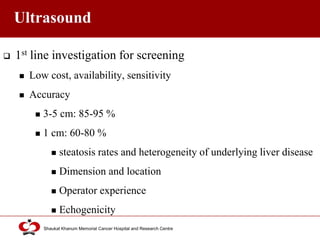
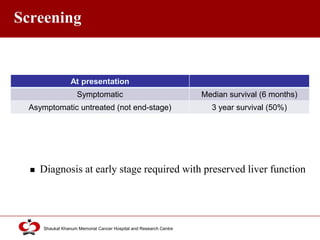
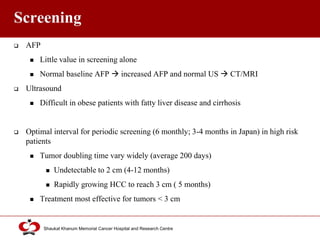
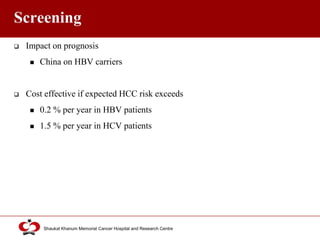
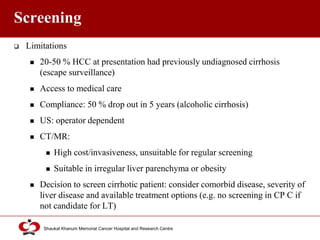
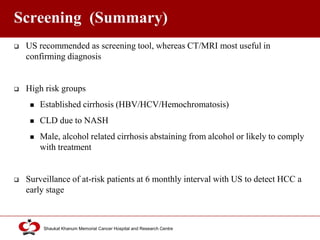
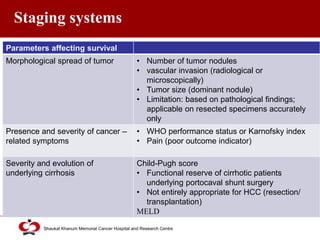
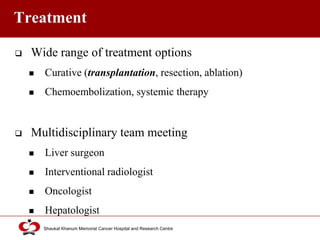
Hepatocellular carcinoma (HCC) is the most common type of liver cancer. Risk factors include cirrhosis of the liver caused by hepatitis B, hepatitis C, alcohol use, and non-alcoholic fatty liver disease. Screening high-risk patients allows early detection when treatment is most effective. HCC incidence varies globally and is increasing due to risk factor epidemics.