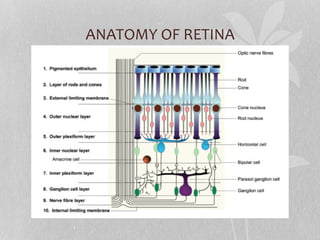
The document summarizes the anatomy of the retina. It describes the layers of the retina in detail and explains conditions like central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO).
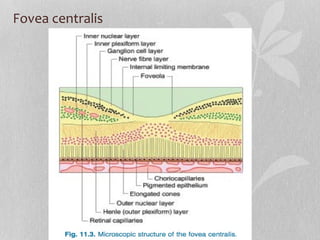
The retina has two main regions - the posterior pole containing the optic disc and macula lutea, and the peripheral retina. The macula lutea contains the fovea centralis, which has tightly packed cones and thin retinal layers. CRAO and CRVO can cause vision loss due to obstruction of the central retinal artery or vein respectively. Management involves treatments like lowering IOP and anti-coagulants.