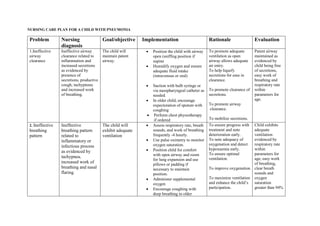
This nursing care plan outlines the diagnosis, goals, interventions, and evaluations for a child with pneumonia across 7 problems:
1) Ineffective airway clearance addressed through positioning, humidification, suctioning, and chest physiotherapy.
2) Ineffective breathing pattern assessed frequently and treated with positioning and supplemental oxygen.
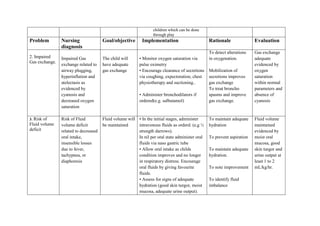
3) Impaired gas exchange monitored via pulse oximetry and treated by encouraging coughing and administering bronchodilators.
4) Risk of fluid volume deficit prevented by IV or NG tube fluids and monitoring intake/output.
5) Altered nutrition addressed with small, frequent meals and encouragement of calorie-rich foods.
6) Fear and anxiety reduced via establishing trust