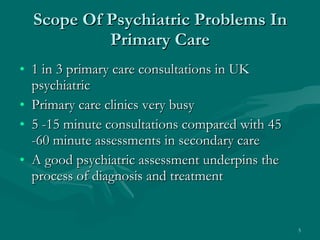
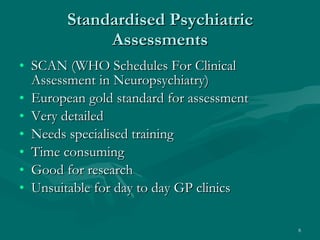
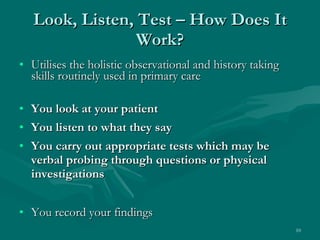
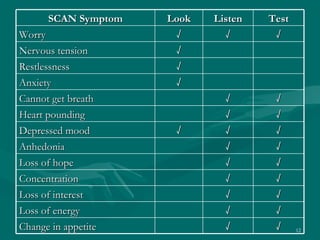
The document discusses mental health assessment in primary care. It introduces the Look, Listen, and Test (LLT) framework for psychiatric assessment. LLT utilizes existing observational and history taking skills in primary care. The physician looks at the patient, listens to what they say, and performs appropriate tests through questions or exams. It can help structure consultations and support a holistic view. The framework draws from the more extensive SCAN assessment but is briefer and more suitable for typical primary care consultations.














![Thank you! [email_address]](https://image.slidesharecdn.com/ivbijaro03-110128095219-phpapp02/85/Ivbijaro-03-22-320.jpg)