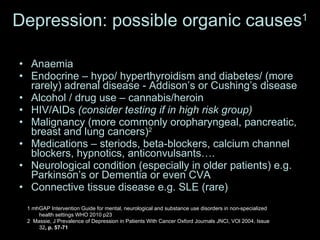
1. Physical examination is important in mental health assessment to identify any underlying organic causes for psychiatric presentations such as infections, metabolic disorders, endocrine abnormalities, and neurological conditions.
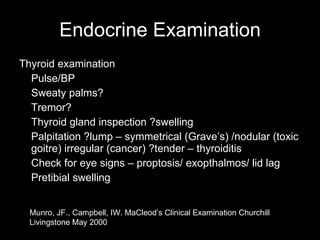
2. The physical examination should be tailored to the particular mental health presentation and may include systems like cardiovascular, respiratory, abdominal, neurological, and endocrine examinations.
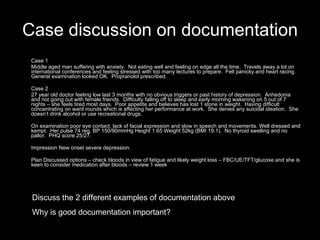
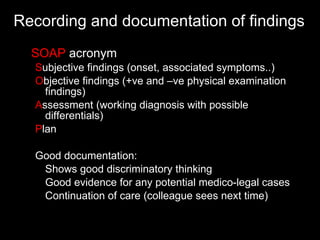
3. Good documentation of physical findings, assessment, and management plan is important for continuity of care, medical-legal purposes, and showing thorough clinical reasoning.


![Anxiety: possible organic causes 1 Chest tightness Angina/MI Asthma Breathlessness PE, COPD, asthma, heart failure, mitral valve disease, pneumothorax Tremor Hyperthyroidism, underlying neurological disorder – Parkinson’s disease, MS… Other organic causes Drugs – antidepressants (SSRI – esp citalopram), stimulants Pheochromocytoma – palpitations, tachycardia, hypertension or orthostatic hypotension, N&V and epigastric pain Rabies – painful laryngeal spasms/dysphagia http://www.wrongdiagnosis.com/symptoms/anxiety/book-causes-5d.htm [website accessed on 2.1.10]](https://image.slidesharecdn.com/harniess01-110124020451-phpapp02/85/Harniess-01-8-320.jpg)
![Psychosis: possible organic causes 1 Infection – cerebral malaria/ sepsis/encephalitis/ meningitis/ HIV/AIDS Alcohol/ drugs withdrawal (heroin, marijuana) Neurological – stroke/ dementia/ Huntington’s chorea Diabetes (especially hypoglycaemia) Electrolyte imbalance (hypo/hypercalcaemia, hyponatraemia, hypomagnesia) Hepatic encephalopathy Brain tumour Medications (e.g. steroids, digoxin, phenytoin, cimetidine, anticholinergic medications) 1 mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings WHO 2010 p32 2 http://www.fpnotebook.com/Psych/Psychosis/PsychsDfrntlDgns.htm [website accessed on 3.1.11]](https://image.slidesharecdn.com/harniess01-110124020451-phpapp02/85/Harniess-01-9-320.jpg)









![Depression screening in chronic Illness 1 2 screening questions During the last month, have you often been bothered by feeling down, depressed or hopeless? During the last month, have you often been bothered by having little interest or pleasure in doing things? 2 1 Ischaemic Heart Disease/ Diabetes/ Cancer/ chronic pain 2 Nice Guidelines Depression October 2009 p17 [www.nice.org.uk]](https://image.slidesharecdn.com/harniess01-110124020451-phpapp02/85/Harniess-01-22-320.jpg)