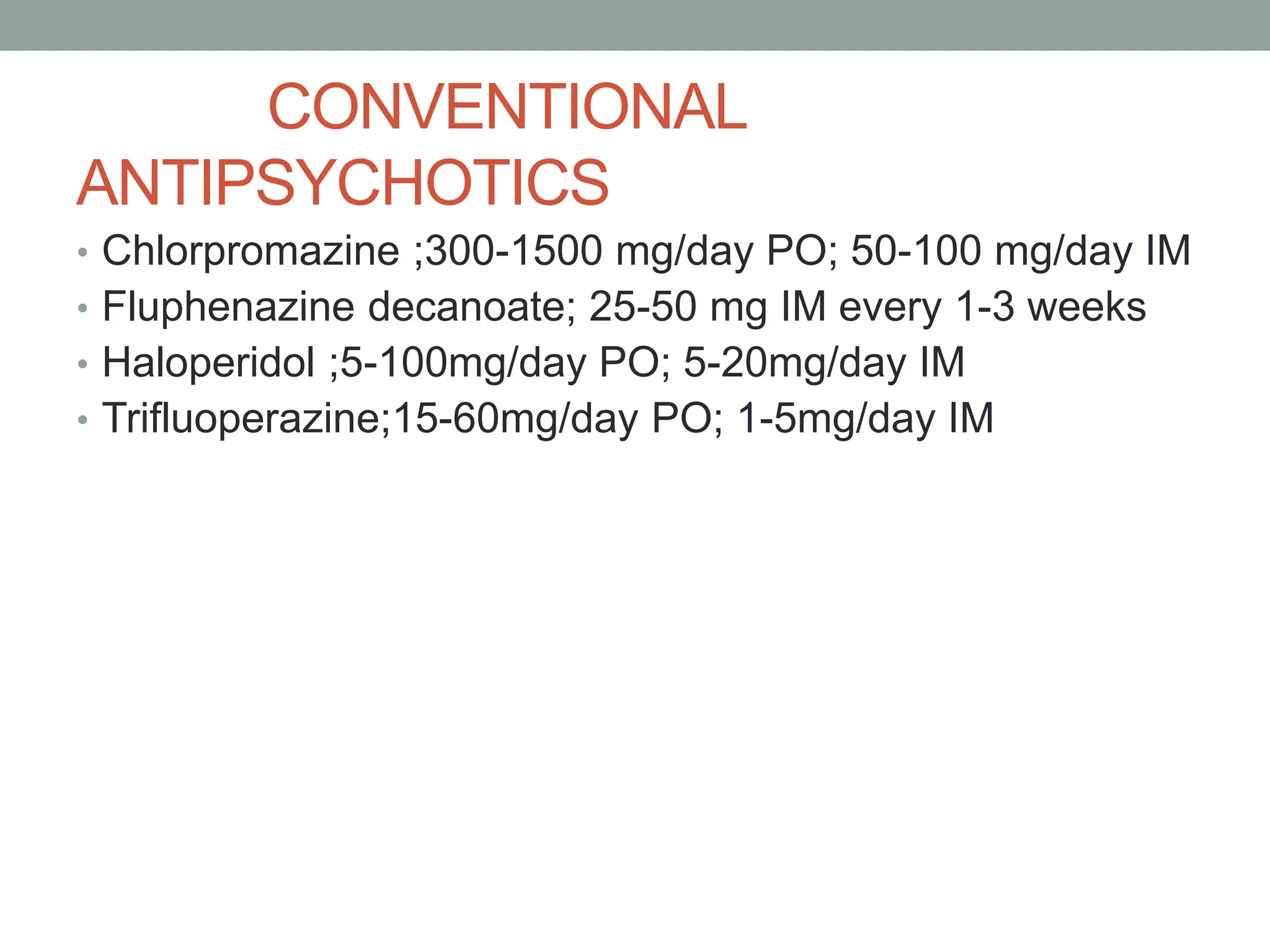
The document provides an introduction to psychiatry and mental health, defining key terms such as normality, mental health, and mental disorders. It details the psychiatric evaluation process, including communication skills and collection of patient history, as well as mental state examinations and the various types of schizophrenia, their symptoms, and treatment options. Additionally, it discusses anxiety disorders, their characteristics, and the distinction between normal anxiety and pathological responses.
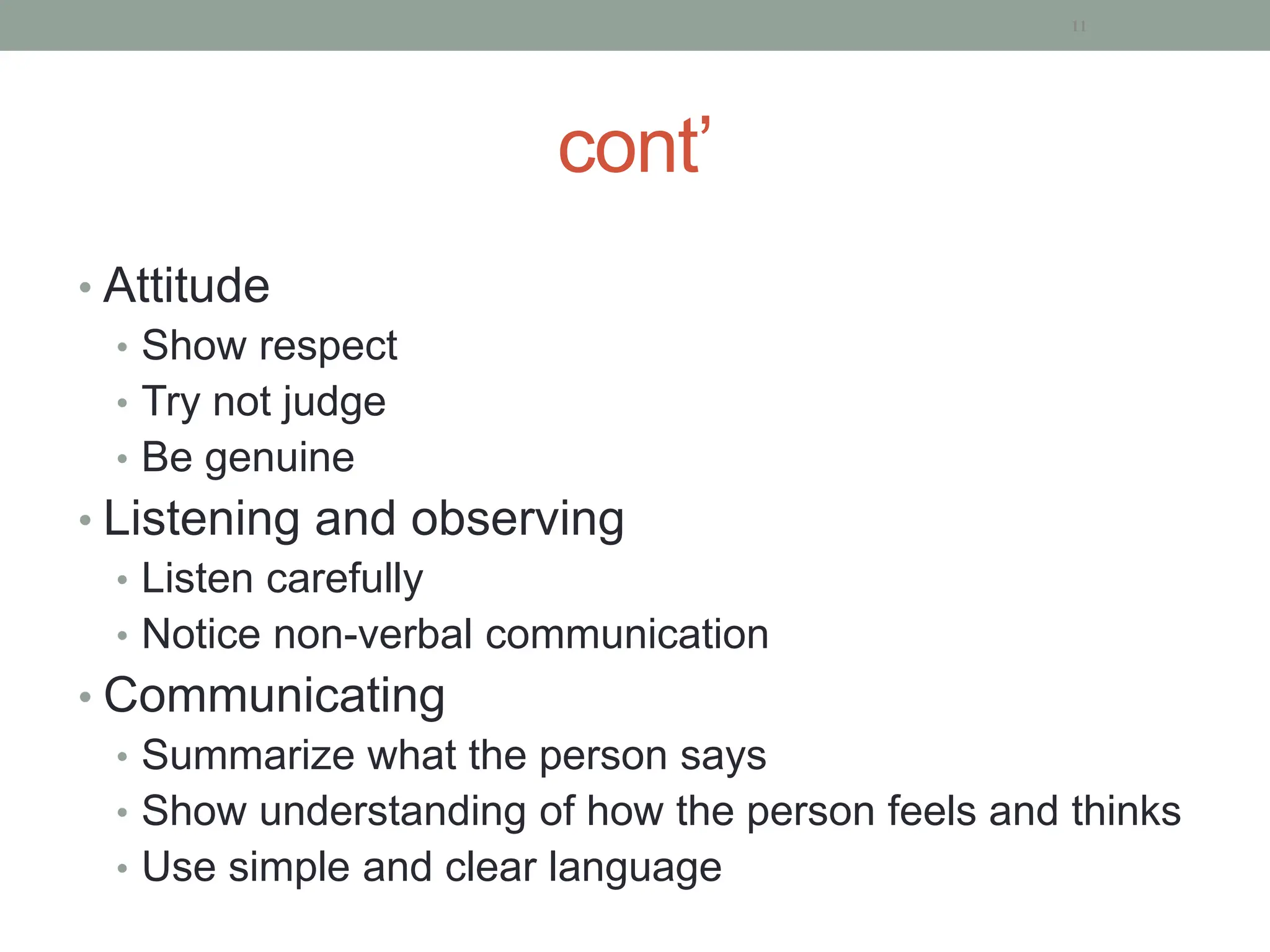
![Schneider’s first rank symptoms of
schizophernia [SFRS]
• He proposed the first rank symptoms of schizophernia in
1959.
• The presence of even one of these symptoms is
considered to be strongly suggestive of schizophernia.](https://image.slidesharecdn.com/2-psychiatricinterview-240322170656-f853b7f9/75/2-Psychiatric-course-for-HO-students-and-other-health-student-67-2048.jpg)
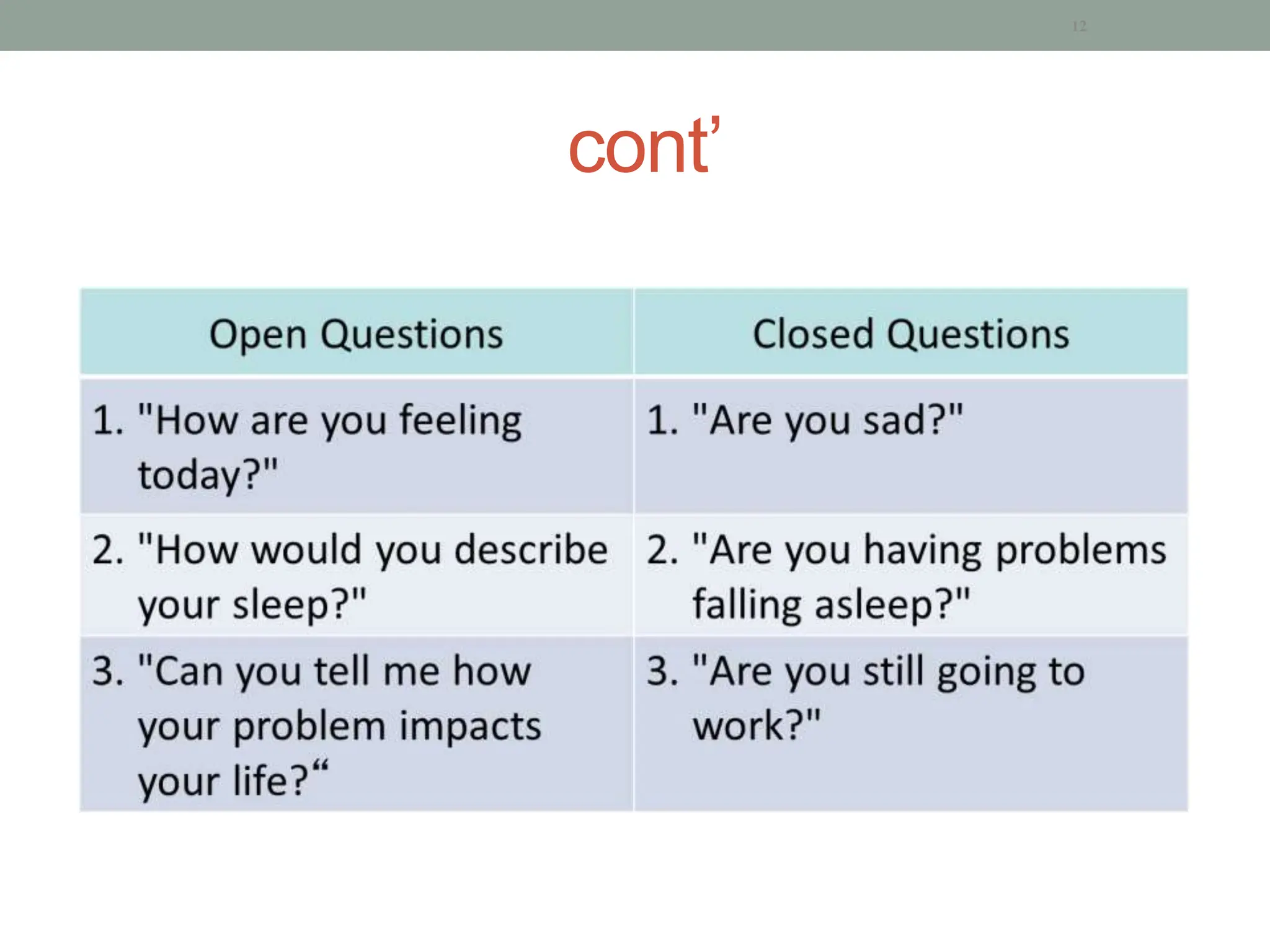
![SFRS
• Hearing one’s thought spoken aloud [audible
thoughts or thought echo ]
• Hallucinatory voices in the form of statement and
reply[the patient hears voices discussing him in the
third person]
• Hallucinatory voices in the form of a running
commentary[voices commenting on one’s action]](https://image.slidesharecdn.com/2-psychiatricinterview-240322170656-f853b7f9/75/2-Psychiatric-course-for-HO-students-and-other-health-student-68-2048.jpg)
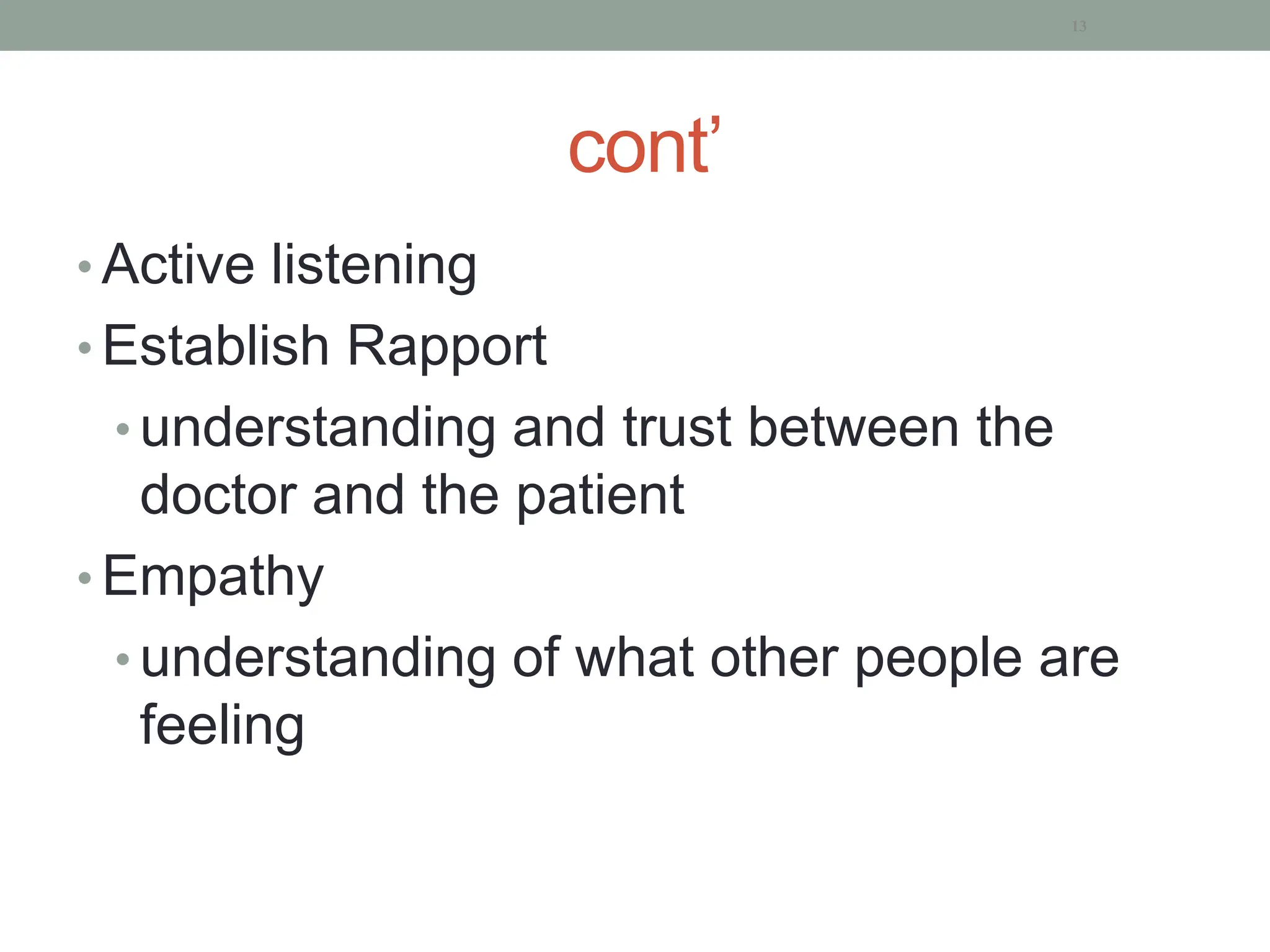
![• Thought withdrawal
• Made volition or acts [the subject being like a robot]
• Made impulse [experiences impulses imposed by some
external force]
• Made feelings [experiences feelings imposed by some
external force]](https://image.slidesharecdn.com/2-psychiatricinterview-240322170656-f853b7f9/75/2-Psychiatric-course-for-HO-students-and-other-health-student-69-2048.jpg)
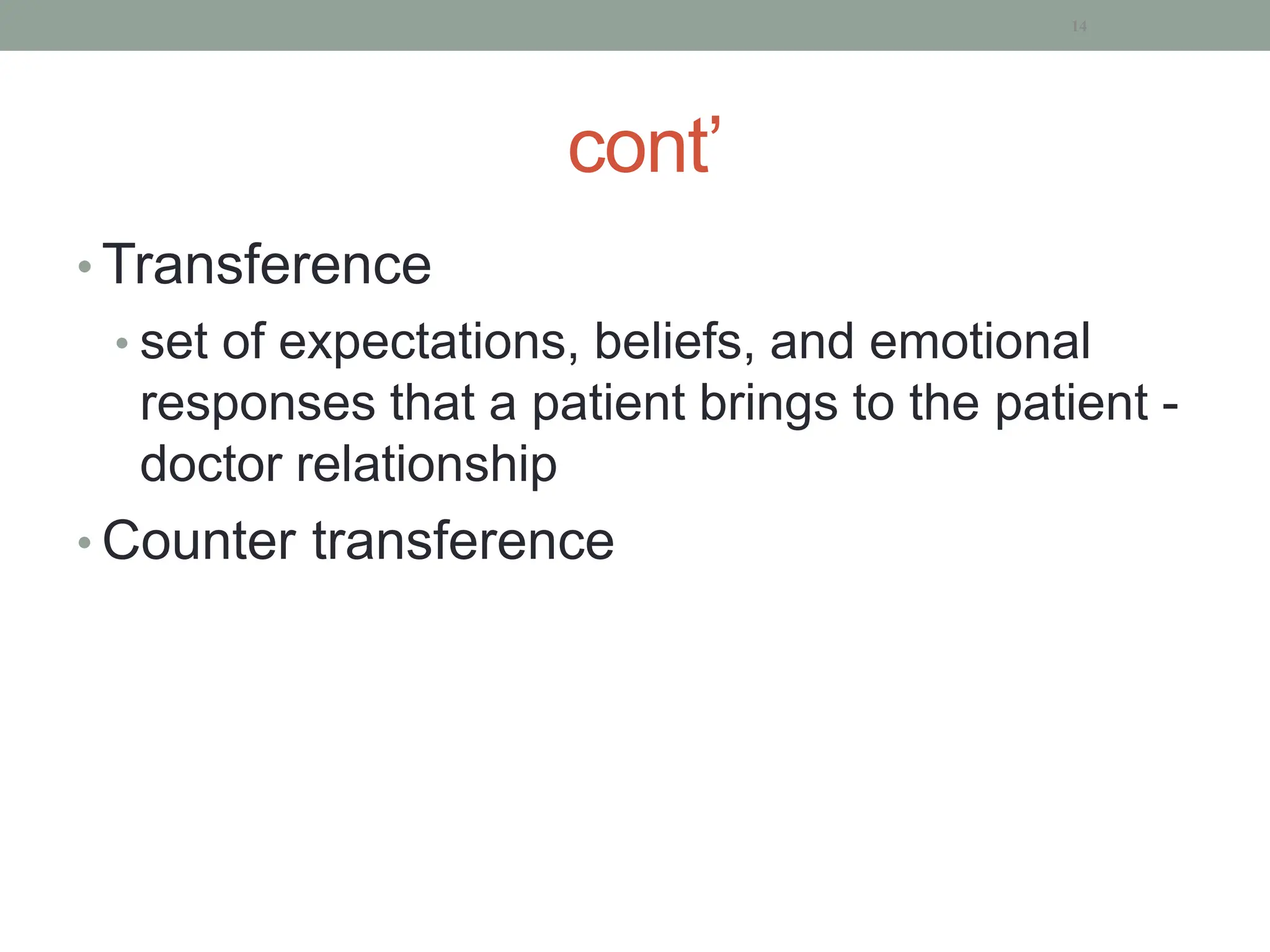
![Course and prognosis
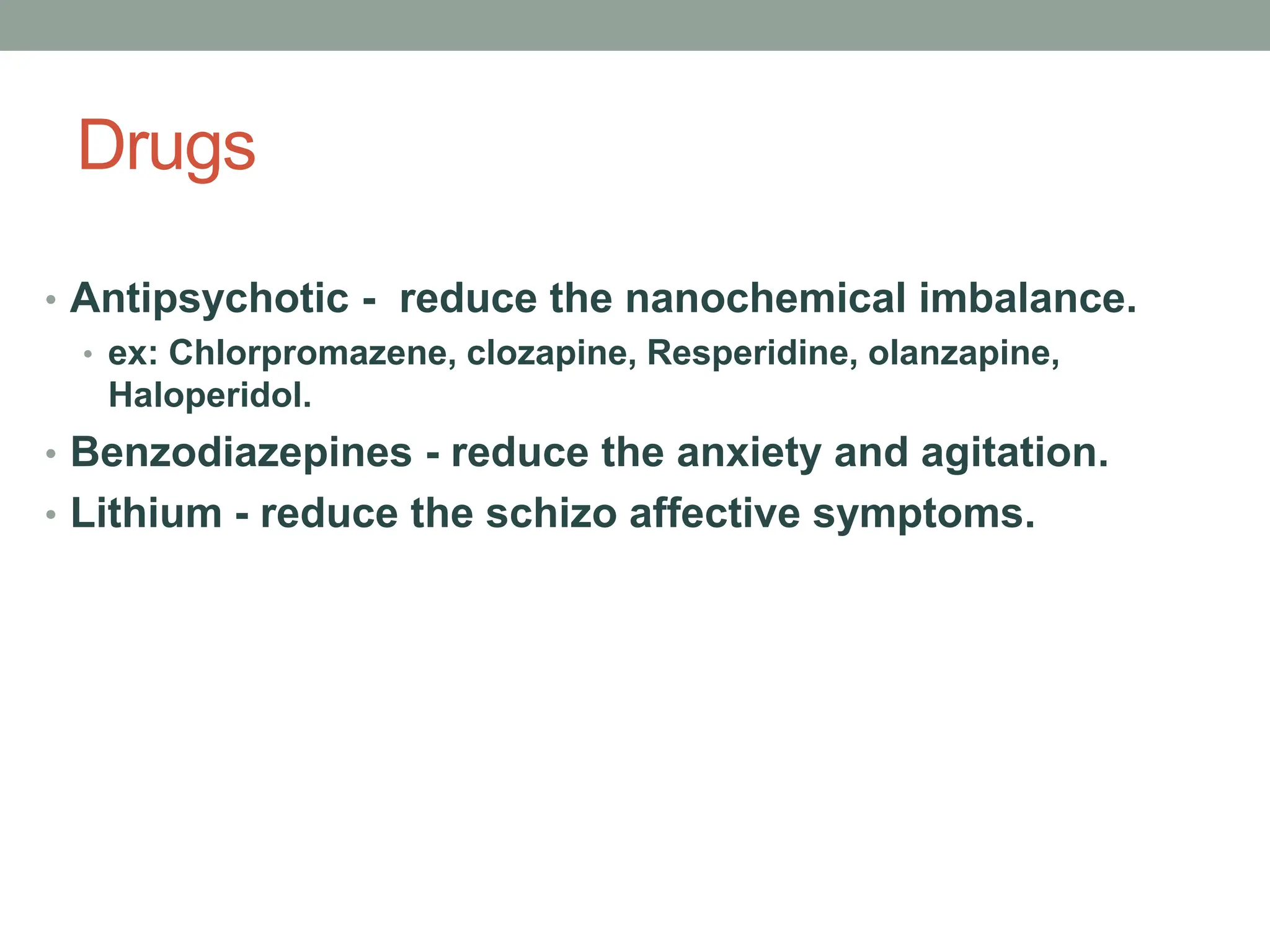
Good prognostic factors Poor prognostic factors
Acute onset
Later onset
Presence of precipitating
factors
Good premorbid
personality
Paranoid, catatonic
Short duration [<6mths]
Chronic
Younger onset
Absence of precipitating
factors
Poor premorbid
personality
Simple, undifferntiated
Long duration[>2yrs]](https://image.slidesharecdn.com/2-psychiatricinterview-240322170656-f853b7f9/75/2-Psychiatric-course-for-HO-students-and-other-health-student-70-2048.jpg)
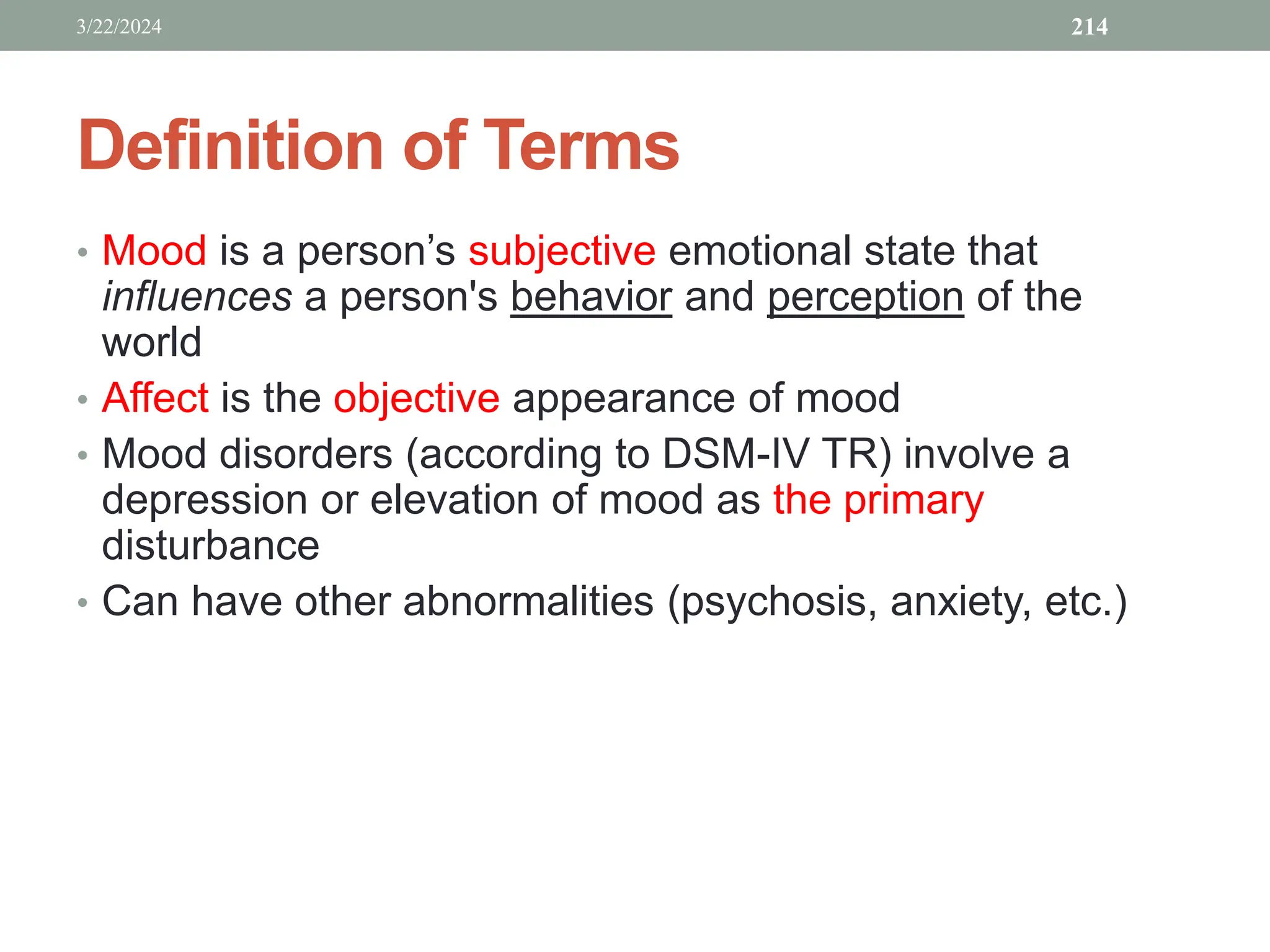
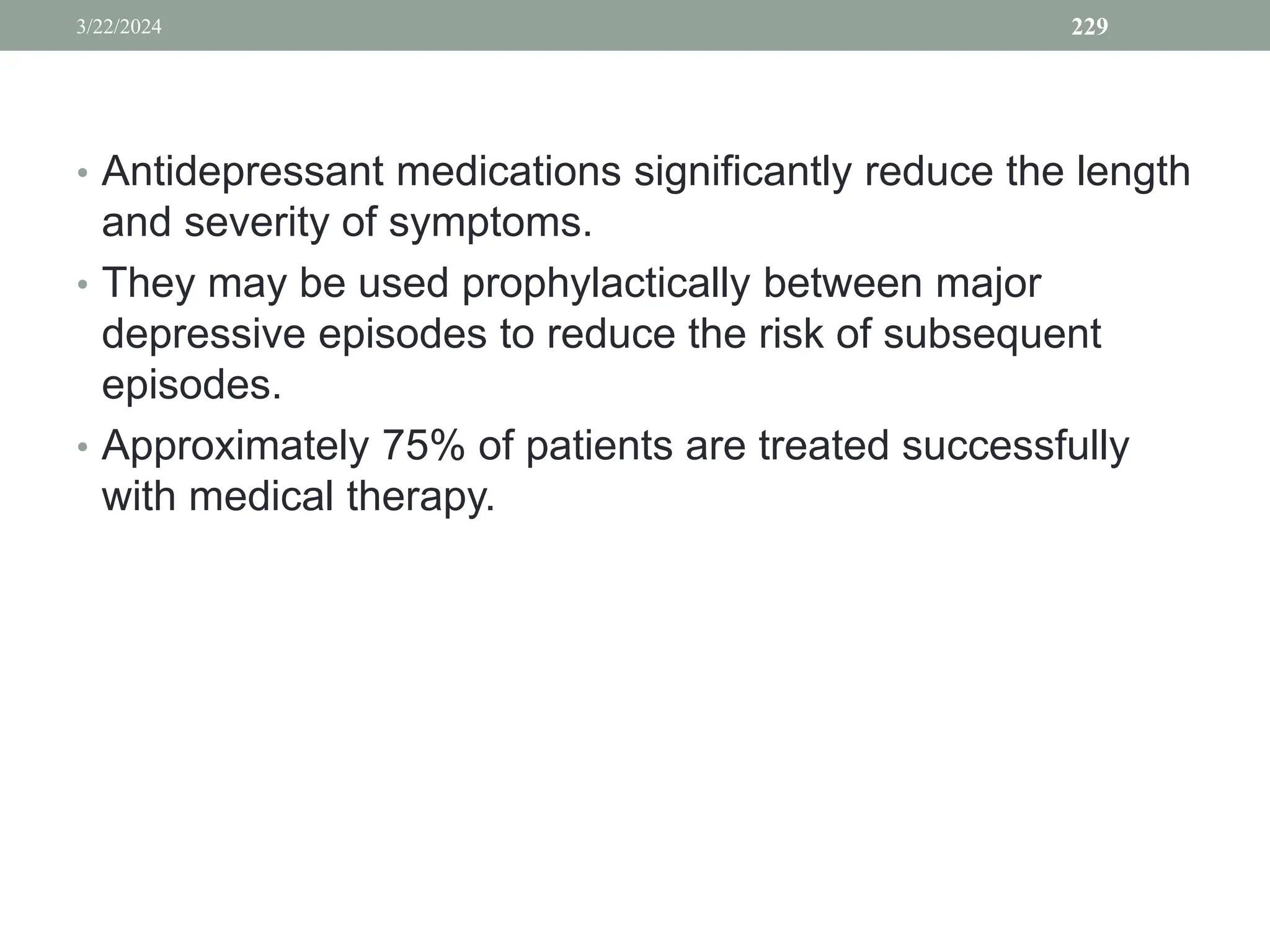
![Epidemiology
• Most common mood disorder
• Point prevalence: 8%–10% females, 3%–5% males
• Lifetime prevalence: 20%–25% females, 8%–13% males,
• Prevalence in Ethiopia 9.1% (only 22% sought treatment)
[Hailemariam, 2012]
3/22/2024 225](https://image.slidesharecdn.com/2-psychiatricinterview-240322170656-f853b7f9/75/2-Psychiatric-course-for-HO-students-and-other-health-student-225-2048.jpg)