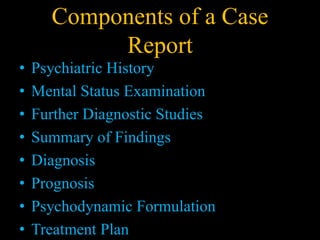
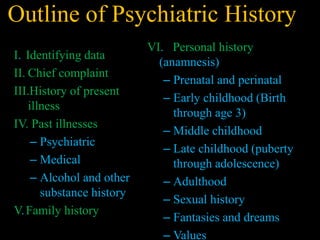
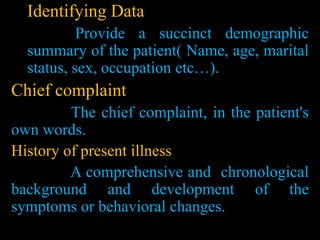
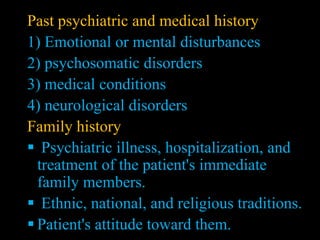
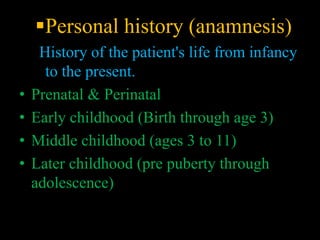
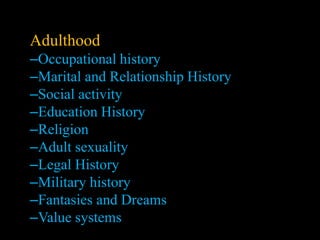
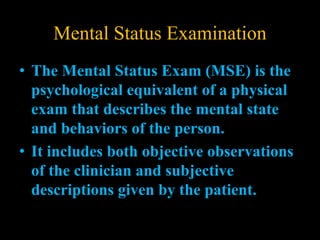
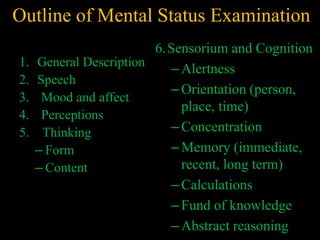
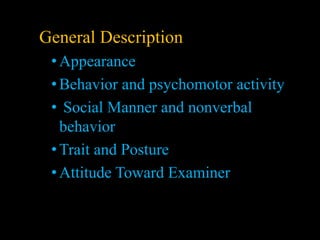
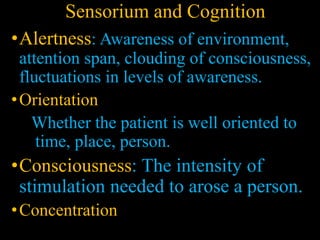
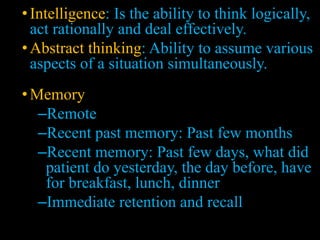
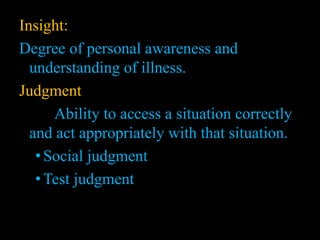
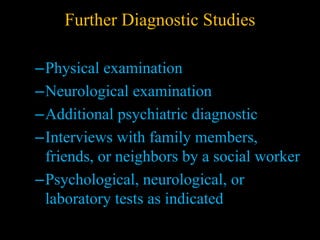
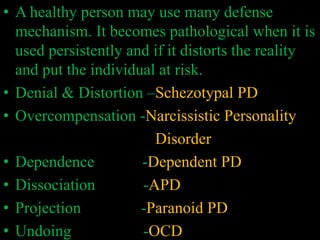
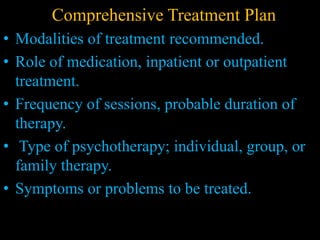
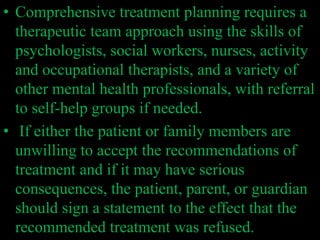
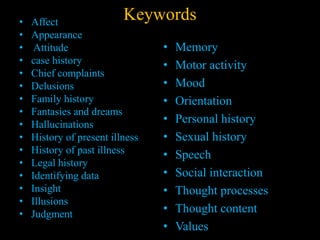
A case report provides a detailed account of a patient's symptoms, diagnosis, treatment, and outcomes. It includes a case history with identifying data, chief complaint, history of present and past illness, mental status examination, diagnostic findings, prognosis, and treatment plan. The case history gathering involves a psychiatric evaluation and psychosocial assessment to understand the patient's symptoms and formulate an effective treatment plan. A comprehensive treatment plan is developed using a multidisciplinary approach to address the patient's needs.