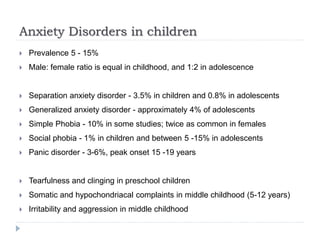
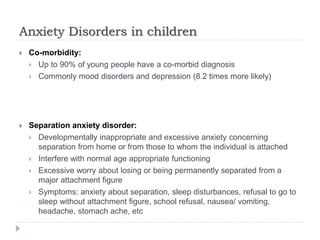
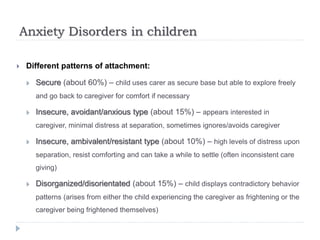
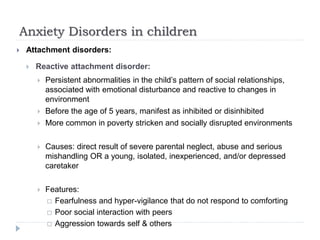
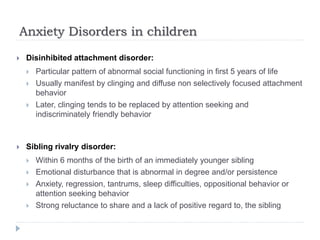
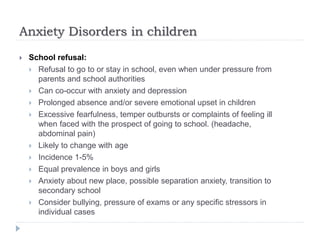
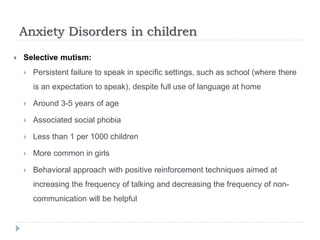
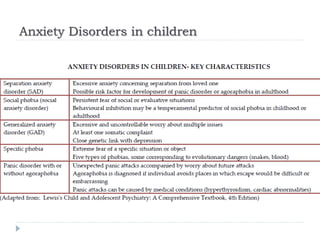
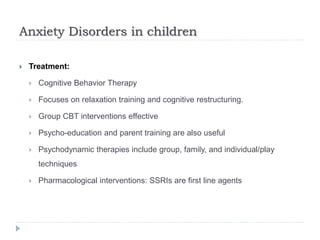
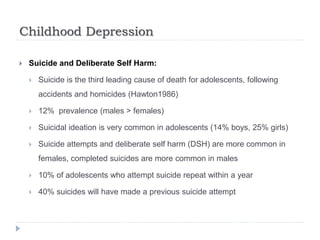
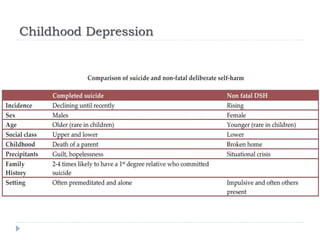
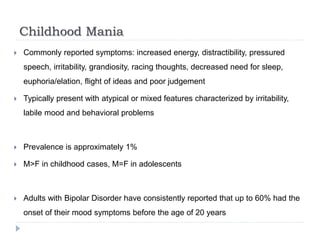
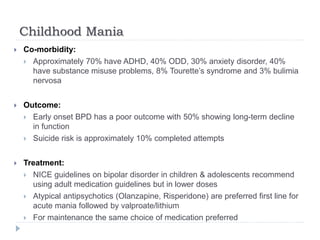
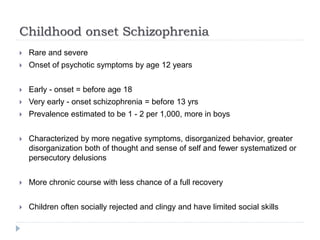
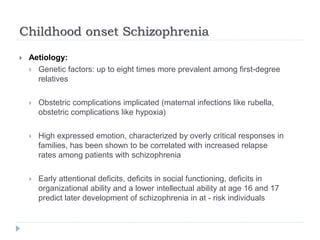
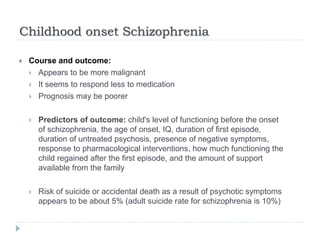
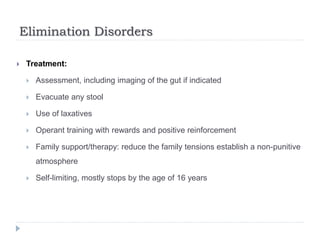
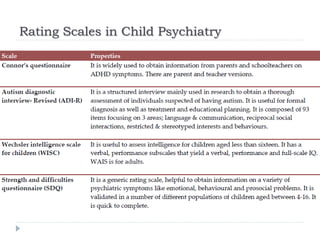
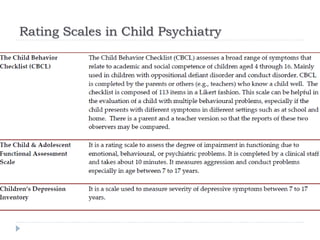
This document provides an outline and overview of various psychiatric conditions that can affect children, including anxiety disorders, depression, bipolar disorder, schizophrenia, and other conditions. It discusses the prevalence, symptoms, risk factors, comorbidities, and treatment approaches for each. Rating scales are also mentioned as a tool used in evaluating children. The document focuses in more depth on anxiety disorders, separation anxiety disorder, attachment disorders, school refusal, selective mutism, childhood depression, childhood bipolar disorder/mania, and early-onset schizophrenia.