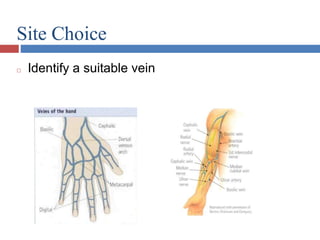
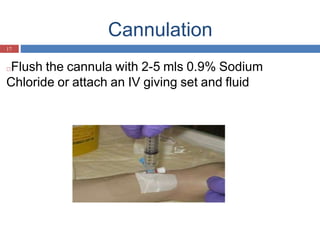
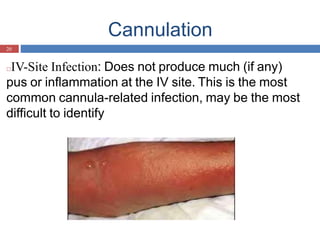
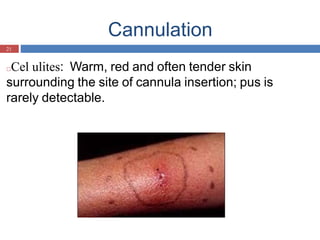
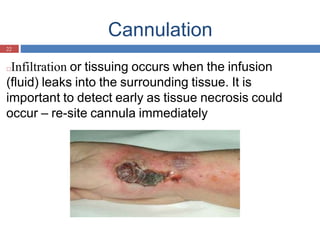
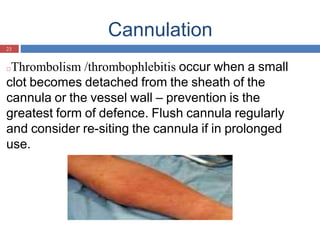
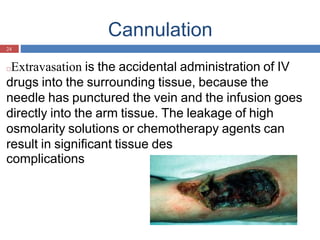
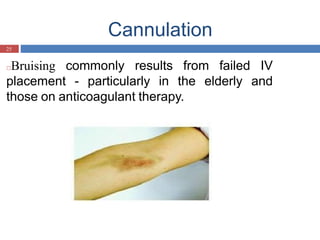
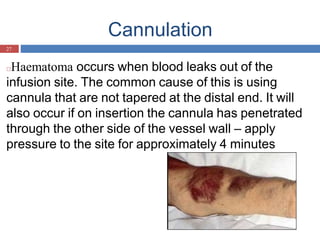
This document outlines the procedure for intravenous cannulation, emphasizing safety, efficacy, and minimizing discomfort. It details indications for use, advantages, necessary equipment, preparation steps, and various techniques involved in cannulation, as well as potential complications that can arise. Additionally, it provides criteria for vein selection and advice on how to maintain and document the procedure effectively.